In what's reported to be a world-first, last Tuesday, a Japanese man received a pioneering retinal cell transplant grown from donor stem cells instead of his own.
Doctors took skin cells from a donor bank and reprogrammed them into induced pluripotent stem (iPS) cells, which can be coaxed to grow into most cell types in the body.
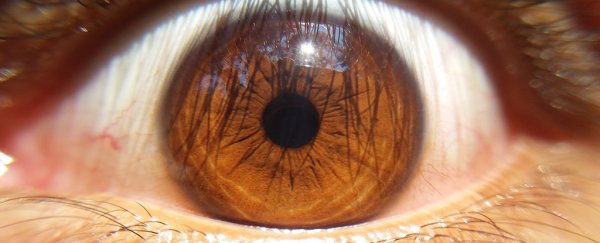
For this procedure, the physicians grew the iPS cells into a type of retinal cell, and then injected them into the retina of the patient's right eye.
The test subject was a man in his 60s who has been living with age-related macular degeneration - a currently incurable eye disease that slowly leads to loss of vision.
If this news sounds somewhat familiar, it's because the same team of Japanese doctors successfully performed a similar transplant in 2014. But in that case, the iPS cells came from the patient's own skin, not from a donor.
The 2014 treatment involved culturing a patient's cells into a thin sheet of retinal pigment epithelium cells, which they transplanted directly under her retina.
One year later, their results showed that the patient's disease had not progressed as it would have without any treatment, and she continues to do well.
But a second case study after the 2014 success never went ahead - the researchers found genetic abnormalities in the iPS cells they had derived from an additional patient's skin. To avoid complications, the doctors from RIKEN and Kobe City Medical Centre General Hospital decided to halt the trial and refine their approach.
Now they are back with a potentially safer technique that uses cells from a donor bank. The patient who received the transplant last week is the first of five approved for a study by Japan's health ministry in February this year. It's important to note that so far this is a safety study - a precursor to a clinical trial.
As team leader Masayo Takahashi from RIKEN told a press conference, we will have to wait and see for several years until we know for sure whether last week's transplant was a complete success - which is the whole point of doing a safety study like this.
"A key challenge in this case is to control rejection. We need to carefully continue treatment," she said.
The patient will be closely observed for a year, and then receive check-ups for three more years. The main things for the team to look out for are rejection of the new retinal cells, and the development of potential abnormalities.
An editorial in Nature praises the team's cautious approach, emphasising that this work with iPS cells could pave a smoother path for other trials in the emerging field of stem cell medicine.
If donor cells turn out to be a viable option in iPS cell procedures, it would be huge for creating more affordable stem cell treatments that anyone can benefit from.
Instead of having to induce stem cells out of each individual patient's samples, doctors could go down the cheaper and quicker route of simply picking a suitable match from a donor bank.
Stem cell treatments such as this new procedure are an extremely promising avenue in medicine, but scientists are right to remain cautious and proceed slowly. Just last month a devastating case report broke the news that three women lost their eyesight by participating in a dodgy stem cell trial.
On the other hand, in 2015, an experimental stem cell treatment showed promise in multiple sclerosis (MS) patients, and just last year, stem cell injections were used to help stroke patients in recovery.
With all these exciting developments, we'll definitely be keeping an eye on further reports from the Japanese team.