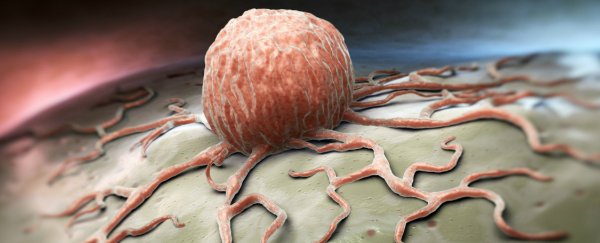
A simple genetic tweak can turn colorectal cancer cells in mice back into healthy tissue in a matter of days, essentially reversing tumour growth, new research has revealed.
The scientists are now looking for ways they can use the same approach to develop more effective and less toxic cancer treatments in humans.
According to a press release put out by the journal Cell, where the research was published: "The findings provide proof of principle that restoring the function of a single tumour suppressor gene can cause tumour regression and suggest future avenues for developing effective cancer treatments."
Most of the drugs we use to fight cancer are designed to kill cancerous cells. While this can be effective, colorectal tumours often come back just weeks after treatment, and the side effects can be intense.
"Treatment regimes for advanced colorectal cancer involve combination chemotherapies that are toxic and largely ineffective, yet have remained the backbone of therapy over the last decade," said senior researcher Scott Lowe from the Weill Cornell Medical College in New York.
But his team may have now found a new way to fight the cancer type, by reactivating a gene known as adenomatous polyposis coli (Apc) that's turned off in 90 percent of human colorectal tumours.
Testing their approach in mice, the team was able to stop tumour growth and restore normal intestinal function within just four days, simply by restoring Apc levels.
Within two weeks, all tumours in the mice's intestines had been eliminated, and six months later there were no signs of the cancer coming back.
While scientists have previously looked into turning certain genes on or off in animal models in order to fight cancer, they've struggled to do so without triggering excess gene activity and causing other problems in normal cells.
But Lowe and his team found a way to precisely and reversibly disrupt Apc activity in a mouse with cancerous tumours in its colon.
They already knew that the Apc gene was closely linked to an important pathway known as the Wnt signalling pathway, which controls cells proliferation, migration and survival. But using their new technique, they managed to show that when Apc is inactivated, Wnt signalling is permanently turned on, and this is what starts the colon cells on a crazy, and ultimately cancerous, growth frenzy.
When the team reactivated Apc in the colorectal cells, Wnt signalling returned to normal levels and the cells stopped proliferating and went back to their normal function.
Within two weeks, the mice's tumours had regressed or disappeared. Even more impressive was the fact that this approach worked on mice with malignant colorectal cancer tumours that contain Kras and p53 mutations - these two mutations are found in about half of all colorectal tumours in humans.
Unfortunately, there is one big barrier stopping this research from working in humans - scientists can't genetically edit humans in the way they can mice. But the researchers are looking into ways they can use drug treatments and other approaches to restore Apc function, or control the overactive Wnt pathway.
"It is currently impractical to directly restore Apc function in patients with colorectal cancer, and past evidence suggests that completely blocking Wnt signaling would likely be severely toxic to normal intestinal cells," said Lowe. "However, our findings suggest that small molecules aimed at modulating, but not blocking, the Wnt pathway might achieve similar effects to Apc reactivation. Further work will be critical to determine whether Wnt inhibition or similar approaches would provide long-term therapeutic value in the clinic."
And while this specific treatment will most likely only work for colon cancer, which kills around 700,000 people worldwide each year, the team believes that the same approach could be tweaked to suit other cancer types.
"If we can define which types of mutations and changes are the critical events driving tumour growth, we will be better equipped to identify the most appropriate treatments for individual cancers," said Lukas Dow, one of the researchers.
We can't wait to see how the research progresses.