Scientists have struggled for millennia to understand human consciousness – the awareness of one's existence. Despite advances in neuroscience, we still don't really know where it comes from, and how it arises.
But researchers think they might be closer to identifying its physical origins, after a study pinpointing a network of three specific regions in the brain that appear to be crucial to consciousness.
Published in November 2016, the research could be a huge deal for our understanding of what it means to be human, and it could also help researchers find new treatments for patients in vegetative states.
"For the first time, we have found a connection between the brainstem region involved in arousal and regions involved in awareness, two prerequisites for consciousness," said lead researcher Michael Fox from the Beth Israel Deaconess Medical Centre at Harvard Medical School back in 2016.
"A lot of pieces of evidence all came together to point to this network playing a role in human consciousness."
Consciousness is generally thought of as being comprised of two critical components – arousal and awareness.
Researchers had already shown that arousal is likely regulated by the brainstem – the portion of the brain that links up with the spinal cord – seeing as it regulates when we sleep and wake, and our heart rate and breathing.
Awareness has been more elusive. Researchers have long thought that it resides somewhere in the cortex – the outer layer of the brain – but no one has been able to pinpoint where.
The Harvard team identified not only the specific brainstem region linked to arousal, but also two cortex regions, that all appear to work together to form consciousness.
To figure this out, the team analysed 36 patients in hospital with brainstem lesions – 12 of them were in a coma (unconscious) and 24 were defined as being conscious.
The researchers then mapped their brainstems to figure out if there was one particular region that could explain why some patients had maintained consciousness despite their injuries, while others had become comatose.
What they found was one small area of the brainstem – known as the rostral dorsolateral pontine tegmentum – that was significantly associated with coma. Ten out of the 12 unconscious patients had damage in this area, while just one out of the 24 conscious patients did.
That suggests that this tiny region of the brainstem is important for consciousness, but it's not the full story.
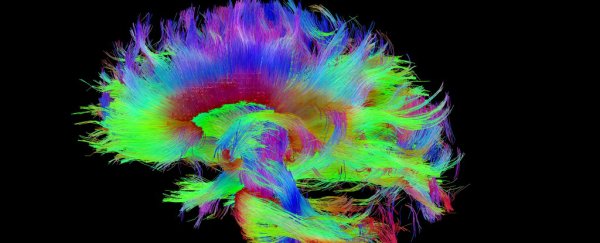
To figure out which other parts of the brain were fully connected to this region, the team looked at a brain map – or connectome – of a healthy human brain, which shows all the different connections that we know of so far in our brains (you can see a connectome in the image at the top of this story).
They identified two areas in the cortex that were linked up to the rostral dorsolateral pontine tegmentum, and were most likely to play a role in regulating consciousness. One was in the left, ventral, anterior insula (AI), and the other was in the pregenual anterior cingulate cortex (pACC).
Both of these regions have been linked by previous studies to arousal and awareness, but this is the first time they've been connected to the brainstem.
The team double-checked their work by looking at fMRI scans of 45 patients in comas or vegetative states, and showed that all of them had the network between these three regions disrupted.
It's a pretty exciting first step, but the researchers acknowledged that they need to verify their find across a larger group of patients.
Independent teams will also need to confirm their results before we can say for sure that these three regions are the physical source of consciousness in our brains.
In the meantime, the research will hopefully lead to new treatment options for patients in comas and vegetative states, who might have otherwise healthy brains but simply can't regain consciousness.
"This is most relevant if we can use these networks as a target for brain stimulation for people with disorders of consciousness," said Fox at the time.
"If we zero in on the regions and network involved, can we someday wake someone up who is in a persistent vegetative state? That's the ultimate question."
The research was published in Neurology.
A version of this article was first published in November 2016.