The majority of women with the most common type of early-stage breast cancer can safely skip chemotherapy after surgery, according to a highly anticipated new report.
The results, released Sunday, are sure to accelerate the decline in chemotherapy for the disease.
The findings came from the largest breast cancer treatment trial ever conducted and showed that most patients who have an intermediate risk of a cancer recurrence - a group that numbers 65,000 women a year in the United States - can avoid chemotherapy and its often debilitating side effects.
"We have been waiting for these results for years," said Allison Kurian, an oncologist at Stanford University who was not involved in the trial. "They are going to change treatment and remove uncertainty for women making decisions."
The same decade-long study had previously confirmed that patients at low risk, as determined by a genomic test of their tumors, can skip chemotherapy.
The two groups, taken together, account for about 70 percent of women diagnosed with the most common type of breast cancer.
That means more than 85,000 women a year can safely forgo chemotherapy.
Some of those women have been skipping chemotherapy based on less rigorous research. Now, they can have confidence in those decisions, experts said.
Other patients may change their treatment approach based on the results of this latest study.
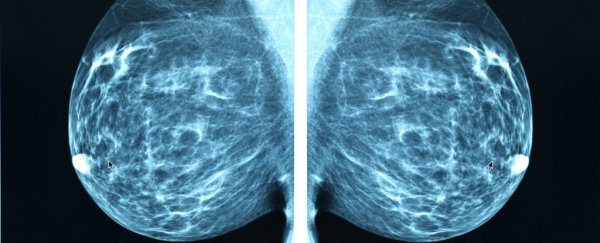
The cancer in question is driven by hormones, has not spread to the lymph nodes and does not contain a protein called HER2.
Generally, after surgery, such patients receive endocrine therapy, such as tamoxifen, which is designed to block the cancer-spurring effects of hormones.
Otis Brawley, chief medical and scientific officer of the American Cancer Society, called the trial a good example of "precision medicine" and said it would save many women from unneeded chemotherapy.
The results came from a federally sponsored trial called TAILORx, which was designed to help doctors more precisely tailor treatments for early-stage breast cancer.
Since 2006, the trial has enrolled more than 10,000 women in the United States and five other countries diagnosed with early-stage breast cancer and followed their progress through post-surgery treatment.
The latest results were presented Sunday morning at the annual meeting of the American Society of Clinical Oncology in Chicago and published in the New England Journal of Medicine.
The patients' tumors were analyzed using a test called Oncotype DX, which examines the activity of 21 genes to predict the risk of a recurrence over 10 years.
Previous studies had made clear that women with low scores could skip chemotherapy and that those with high scores should get it.
The big outstanding question was: What should women with midrange scores get? Such patients have been in "the gray zone, and we haven't known what to tell them," Kurian said.
To find the answer, researchers randomly assigned more than 6,700 women with intermediate scores - 11 to 25 - to two groups. After surgery, one group got endocrine therapy only, while the other was treated with endocrine therapy plus chemotherapy.
After years of follow-up, the data showed that most patients who did not get chemotherapy fared as well as those who did.
Women age 50 or younger were the notable exception.
Those with recurrence scores of 16 and above got a "substantial" benefit from chemotherapy and should consider it, said lead author Joseph Sparano, associate director for clinical research at the Albert Einstein Cancer Center and an oncologist at Montefiore Medical Center in New York.
Phyllis Laccetti, a 58-year-old night nurse at Montefiore, was diagnosed with cancer in her right breast in 2007. She had a lumpectomy, followed by a mastectomy, and had a recurrence score of 12 or 13, which put her in the middle range.
She enrolled in the TAILORx trial and was relieved to be randomly assigned to the group that did not get chemotherapy. She got only tamoxifen.
Because of her work as a nurse, she was familiar with chemotherapy's sometimes harsh effects. She also watched her brother and sister - who died of thyroid cancer and leukemia, respectively - suffer through chemotherapy treatments.
"They were sick all the time," she said. "My brother was so sick that he'd be saying, 'I can't do this anymore,' and it was the same thing with my sister."
Laccetti's cancer has not returned.
The trial results are the latest piece of the puzzle on how to treat early-stage breast cancer. Most patients with the disease have a high survival rate, but their prognoses worsen drastically if their cancer returns in other parts of the body.
Because of that, many women with early-stage cancer used to be urged to get chemotherapy in hopes of preventing any spread.
But in recent years, as many doctors concluded that women with early-stage cancer were being overtreated, they have reduced their use of chemotherapy, which can cause nausea, fatigue and, in rare cases, more serious complications such as leukemia and heart failure. Oncotype DX has spurred the trend and is likely to accelerate it.
Yet the move away from chemotherapy has been hotly debated, with some doctors warning that chemo can save lives and that a "de-escalation" of treatment could be dangerous.
James Doroshow, director of the cancer treatment and diagnosis division at the National Cancer Institute, which was the primary sponsor of the study, predicted that the trial would lead to changes in treatment "for a large number of potential patients." He expects treatment guidelines to quickly change based on the study, which was conducted by a research group named ECOG-ACRIN.
He added that it was important that the federal government funded the study because the pharmaceutical industry has little interest in sponsoring trials that result in a reduction of treatment.
Other experts said the results confirm what many patients and doctors are already doing.
"Oncologists have been getting much smarter about dialing back treatment so that it doesn't do more harm than good," said Steven Katz, a University of Michigan researcher who examines medical decision-making.
"That's important because chemo is toxic; it whacks patients out and can result in long-term job loss."
In a paper published in December, Kurian and Katz reported that chemotherapy use was plunging among patients with early-stage breast cancer.
Their study showed, for example, that chemotherapy use in patients whose cancer had not spread to the lymph nodes declined from 26.6 percent in 2013 to 14.1 percent in 2015.
Harold Burstein, a breast cancer specialist at Dana-Farber Cancer Institute, said that in some ways the debate over de-escalation misses a larger issue.
"You want to bring the right amount of treatment to the tumor based on its biology," he said. "It's not the size of the hammer, it's whether it's the right tool for the job."
While chemotherapy is being dropped for some cases, it's being increased for more aggressive cancers. "We want to give the right amount," he said. "No more, no less."
2018 © The Washington Post
This article was originally published by The Washington Post.