Not all surgical incisions are the same. While a typical straight cut might be preferred by some, a zig-zagging path can reduce scar tissue, making it a preferred method for some cosmetic procedures.
An investigation by researchers at Nanyang Technological University, Singapore (NTU Singapore) has found cellular differences between the two methods, which could lead to more effective surgical incisions.
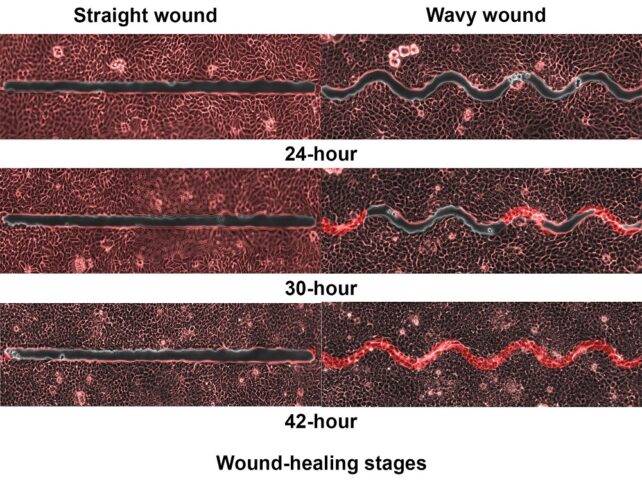
Monitoring of simulated wound healing in biosynthetic materials over 64 hours found that wavy gaps in fact heal nearly five times faster than straight-edged ones, thanks to distinctions in the cells' movement pathways.
"Scientists have long known that the way you cut your skin affects how fast it heals," says mechanical engineer K Jimmy Hsia from NTU Singapore.
"However, not much is known about why this happens and the factors that could affect the healing speed."
Adding to scientists' understanding of the processes in wound healing pathways, Hsia and his team studied how Madin-Darby canine kidney (MDCK) cells close gaps in wounds they created with cuts on a skin created from a micropatterned hydrogel.
The epithelial cells they used from dog kidneys are the same type as those in human skin. Epithelial cells make up the structural tissue that forms our external skin and lines our internal organs. Embryonic development, tissue repair, and wound healing all rely on these cells' ability to seal off gaps in tissue.
The scientists used a method for measuring the movement of fluids called particle image velocimetry to watch MDCK cells work near the 30 to 100 micrometer-wide cuts.
The wavy cuts had a radius of curvature of either 50, 75, or 100 micrometers. They paid special attention to how the width and curvature of the cuts affected the process.
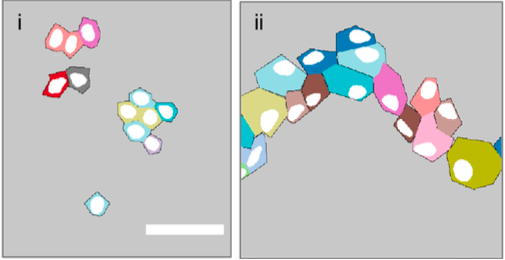
"The highly nonuniform and rotational motion induced by wavy wounds allowed more opportunities for cells to move around, compared to straight wounds," biomechanical engineer Xu Hongmei says.
Cells near the straight wounds moved along the edges, while wavy wounds made cells move in a swirl that resembled a vortex.
"This enabled cells to quickly connect with similar cells on the opposite site of the wound edge, forming a bridge and closing the wavy wound gaps faster than straight gaps," Xu explains.

The range of curvature didn't have a significant effect on speed of healing in wavy wounds, but width needed to be small enough to form bridges. The experiments showed success with a maximum gap size of 75 micrometers.
The team notes this top distance may be different for different cell types, and there could be an effect on bridge formation and healing speed if the curvatures are smaller or larger than the ranges they used.
However even in the smallest experimental gap of 30 micrometers, the cells mostly moved parallel to – and rarely towards – the straight cuts. And they didn't form bridges.
Hsia and colleagues considered if the bridge formation could have been helped by wavy edges causing more cells to divide and grow, increasing the number of cells available for healing, but calculations ruled this out.
"Observations clearly demonstrate that straight and wavy edges provided different geometric confinements to cell migration," they write in their paper, "generating different cell movement patterns …thus different healing efficiency".
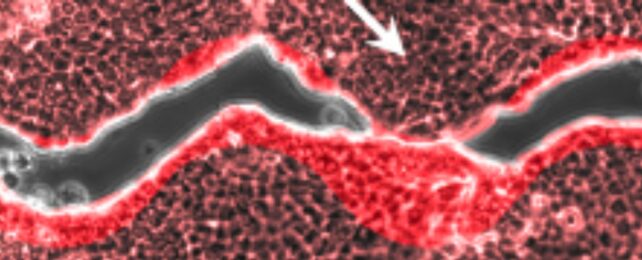
Another thing the researchers noticed was the position of the cell nucleus. In cells not involved in healing a wound, it was roughly in the middle. Yet in cells over the healed gaps it was clearly off center, seeming to move closer to the cell edges to avoid sitting directly over the gap. This was more noticeable in cells over the wavy wounds.
They suggest this indicated the cells that closed wound gaps were under a lot of mechanical tension, and the cells near zig-zagged wounds were more stretched than those over the straight lacerations.
"This study has revealed the cellular and molecular mechanisms of gap closure, contributing to the scientific understanding of the underlying principles of the wound-healing process," mechanical engineer Huang Changjin concludes.
"Clinicians and surgeons can use this knowledge to develop better strategies, such as incision methods, for patients' wound management care in future."
The research has been published in the journal Proceedings of the National Academy of Sciences.