Even once a person gets sick with a coronavirus that's no guarantee they won't contract it again, new research suggests.
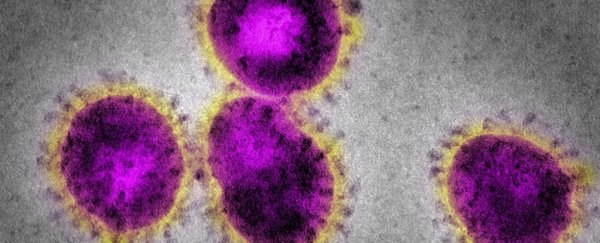
While SARS-CoV-2 is the coronavirus that has the world's attention right now, there are numerous others that we've known about for decades, which are not only known to infect humans, but are highly seasonal.
Researchers have studied four species of these seasonal coronaviruses across the past 35 years, and found reinfection occurred frequently, around a year after the first bout.
While that doesn't necessarily say anything about the current global pandemic, it's not a good sign for the hope of long-term immunity in a population.
Analysing 513 serum samples collected since the 1980s from 10 healthy males living in Amsterdam, researchers noticed several spikes of an antibodies linked to coronaviruses.
Each of these spikes was interpreted as a reinfection, and for all four seasonal coronaviruses studied - including HCoV-NL63, HCoV-229E, HCoV-OC43, and HCoV-HKU1 - the team found three to 17 infections per patient.
Some rare reinfections showed up as early as six months after initial infection, but more frequently, they came back about a year after, "indicating that protective immunity is only short-lived."
To date, there are few confirmed cases of COVID-19 reinfection, but many have faced dispute as it's still too early to say how long acquired immunity to SARS-CoV-2 can last.
Looking to other coronaviruses is one of our best clues, and unfortunately, this 35-year study suggests immunity for many coronavirus infections is not only temporary, it's short-lived. What's more, the authors say reinfection may be a common feature of all human coronaviruses.
The study is limited in that antibody levels act only as a proxy for coronavirus infections - we can't say for sure that each uptick in antibodies was definitely another reinfection.
The research was also done on a small sample of participants, so larger cohort studies are needed.
That said, it does have some perks that other research doesn't.
"Our serological study is unique because it avoids the sampling bias of previous epidemiologic studies based on symptoms-based testing protocols," the authors of the new study write.
Instead, patients were regularly tested, multiple times a year over several decades, even when they were feeling healthy. This is important as many coronavirus infections can remain asymptomatic, which means we could be overlooking many reinfections.
Recent research, specifically on SARS-CoV-2, indicates that specific antibody levels begin to decrease within the first 2 months after infection, especially after mild cases (which is what most people get).
The new study found a similar timeline.
Blood samples, which were collected every 3 months before 1989 and every 6 months after (bar an unexplained six-year gap in the data), show most coronavirus infections in Amsterdam occurred in winter.
"In our study, the months of June, July, August, and September show the lowest prevalence of infections for all four seasonal coronaviruses," the authors write, "confirming the higher prevalence in winter in temperate countries, and SARS-CoV-2 might share this feature in the post-pandemic era."
This is similar to research on other human coronaviruses, which show infection rates slowing in summer.
With the Northern Hemisphere now firmly in fall, that's an extremely worrying result if the new findings apply to the current global pandemic.
Whether SARS-CoV-2 follows the same trend as other coronaviruses remains to be seen. But if we want to be as careful as possible, we should not assume long-term immunity is a thing, because in the end, relying on vaccinations and natural immunity may only get us so far with this virus.
Acquiring a long-lasting immune response from a vaccine could be difficult. It might be that we have to get regular updates, like we do with the seasonal flu.
The study was published in Nature Medicine.