If you have access to it, it's easy to take today's contraception for granted. But key discoveries over the last century or so changed the lives of women.
Before the invention of modern intra-uterine devices (IUDs) or hormonal contraception, most products had low effectiveness, and were more useful for delaying pregnancy than preventing it.
When the contraceptive pill became available in the early 1960s, it marked a turning point. Its very low failure rate of less than 1 percent when used properly, helped put control of contraception firmly in women's hands.
While the pill can have some serious side-effects, for many women it still provides a much less uncomfortable experience than many of the methods that preceded it.
1. Reusable condoms
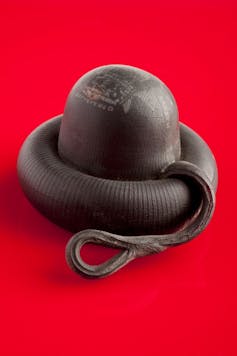
People have used sheaths since at least the 17th century, mostly to prevent sexually transmitted infections. Initially these were made of natural material such as animal intestines or linen.
Just a few years after the invention of synthetic rubber (1844), the rubber condom was created. It was designed to be rinsed and re-used, but as a result it was thicker and less comfortable than today's male condoms.
The disposable latex condom was not invented until the 1930s. These were thinner, more comfortable and, of course, used only once.
Later that decade, US courts overturned a ban on the sale of "immoral goods", which helped make condom use more widespread.
2. Acid-soaked sponges
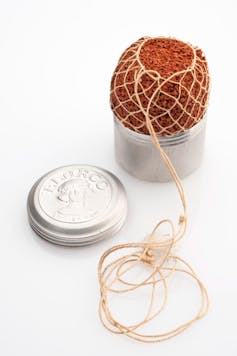
Since acid kills sperm, one traditional home-made method of contraception involved inserting a vinegar-soaked sponge into the vagina. Purpose-designed sponges became commercially available at the beginning of the 20th century and contained chemical spermicide.
Variations of the spermicidal sponge are still available. However, less than 1 percent of women in the UK use the sponge today.
The typical failure rate, particularly for young women, is about 12 to 24 percent per year. In general, younger women are more likely to get pregnant while using less effective methods because they are more fertile than older women.
3. Diaphragms and caps
Diaphragms and their smaller cousins, called caps, were invented in the early 19th century.
Like condoms, they work as physical barriers to sperm, and like sponges are also used with chemical spermicide. They are inserted before sex into the vagina and should stay in place for a least six hours afterwards to allow the spermicide to kill sperm.
The cap and diaphragm were widely used in the US and Europe before the second world war. But the typical failure rate for young women using these methods is about 12 percent. Partly as a result, less than 1 percent of women worldwide use them today.
The high failure rates of barrier methods are partly because they don't stop women ovulating. If sperm manage to get through the barrier, the chances of fertilisation are high.
The other drawback is that they are difficult to fit and must be in place before sex, at a time the woman would probably prefer to be thinking of other things.
4. Douching with antiseptic
Rinsing the vagina after intercourse, often with antiseptic solution, was used as contraception in the early 20th century. Douching does not affect sperm which has already started on its journey through the cervix. So the efficacy of vaginal douching was very low.
Today health professionals strongly discourage douching because of the harm it does to vaginal flora (the natural protective bacteria in the vagina), which can lead to vaginal irritation and infection.
5. Silkworm gut IUDs
Intra-uterine devices (IUDs) remain popular but they didn't always work the same way as modern products.
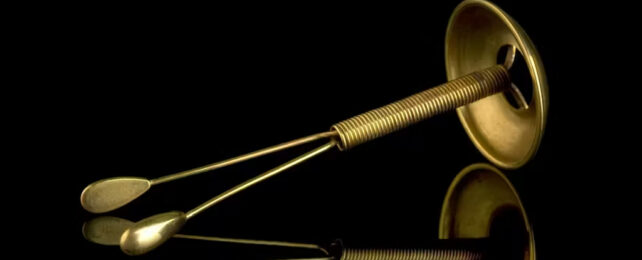
Early intrauterine methods worked on the (partially correct) belief that any device sitting inside the womb is likely to stop a fertilised egg from implanting and developing in the womb. In the 19th century, wishbone pessaries (so called because of their shape) were used to prevent pregnancy.
These devices had two arms which protruded through the cervix into the vagina, and a button ending which covered the cervix. It is hard to imagine that these were comfortable.
Polish gynaecologist Richard Richter published a paper in 1909 about how he inserted a ring of silkworm gut into a patient's womb, with two protruding strings to allow removal. At the time a lot of gynaecologists were discreetly using their own versions of such devices, because of laws against promoting contraception in many countries.
The Graefenberg ring replaced the silkworm gut with a metal alloy ring in the 1920s. German gynaecologist Ernst Graefenberg first tried pure silver, but the body absorbed it and turned the women's gums blue.
All kinds of materials and shapes of IUDs, from leaf shapes to spirals, were used throughout the fifties, sixties and seventies until researchers realised copper improved the effectiveness of the devices.
By the 1970s there were about 70 different intra-uterine devices on the market in the USA.
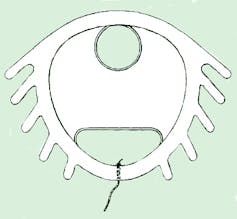
But one of these copper coils, the infamous Dalkon shield, allowed bacteria to ascend into the womb, because of the design of the threads used to retrieve it. This was responsible for high numbers of infections and made acceptance of intrauterine methods plummet in the 1970s.
Modern intrauterine devices (IUDs) sit fully in the womb, contain either copper or slow-release progesterone-type hormones, and are much safer and more effective than older devices.
Infections due to IUDs are rare now but occasionally happen in the first few weeks after insertion. Both hormonal and copper coils now have failure rates of less than 1 percent.
We now have several methods of contraception which, if used correctly, rarely fail, but women still struggle to find a method that suits them. New research is focused on reducing the side effects of contraception but in the meantime governments should invest in sexual health services to give people better, faster access to contraceptives and advice to choose the method that suits them best.![]()
Susan Walker, Reader in Contraception, Reproductive and Sexual Health, Anglia Ruskin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.