Many people who are genetically predisposed to type 1 diabetes never get the disease, hinting at an unknown environmental trigger could play a role in the development of this chronic autoimmune condition.
While some speculate the trigger could be a virus, a new study led by researchers from Cardiff University in the UK points in a different direction: Type 1 diabetes might start with proteins on bacteria, sparking an ominous shift in the immune system.
"Type 1 diabetes is an autoimmune disease that usually affects children and young adults, where the cells that produce insulin are attacked by the patient's own immune system," explains lead author Andrew Sewell, an immunologist at Cardiff University's School of Medicine.
"This leads to a lack of insulin, meaning that people living with type 1 diabetes need to inject insulin multiple times a day to control their blood sugar levels," he says.
Insulin helps glucose move from the bloodstream into our cells, which use it for energy. It's a vital hormone produced by beta cells in the pancreas, and without it, the body's blood sugar can surge to dangerously high levels.
In previous research, Sewell and his colleagues linked the loss of insulin-producing tissues with killer T cells – a class of white blood cells that kill certain other cells, including cancer cells or cells infected by a pathogen. Killer T cells seem to play a key role in causing type 1 diabetes by killing beta cells.
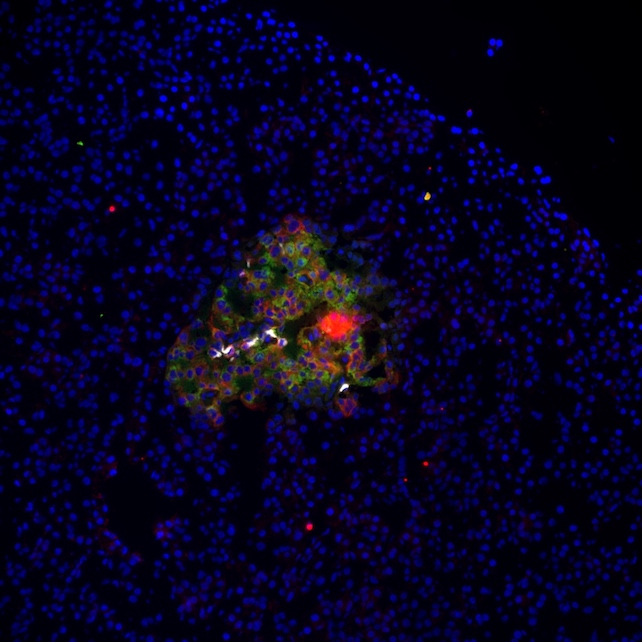
In the new study, the researchers found that killer T cells begin doing this when activated by bacterial proteins; specifically proteins from bacteria known to infect humans, like Klebsiella oxytoca.
The team conducted lab experiments to simulate such infections, introducing bacterial proteins to cell lines from non-diabetic human donors and observing how the donors' killer T cells reacted.
"We found that after encountering proteins from some infectious bacteria, killer T cells could mistakenly also kill cells producing the insulin protein," Sewell says.
"We found activated T cells with this same 'cross-reactivity' in the blood of patients with type 1 diabetes," he adds, "suggesting that what we saw in laboratory experiments could have triggered the disease."
Strong interaction with bacterial proteins apparently initiated this change in killer T cells' behavior, notes Lucy Jones, the chief clinical investigator for the study at the Cardiff University School of Medicine.
The team observed this in relation to a gene for a protein on our own cells called a human leukocyte antigen (HLA) which allows our immune system to tell our own tissues apart from intruders.
"The specific HLA associated with the bacterial infection that triggers diabetes is only present in around 3 percent of the population in the UK," Jones says. "So the bacterial pathogens that can generate anti-insulin T cells are caused by a rare infection in a small minority of people."
By demystifying the origins of type 1 diabetes, the researchers say, we may reveal new ways to treat the disease – or maybe even learn how to prevent it.
"We hope that understanding how T cells trigger diseases like type 1 diabetes will allow us to diagnose and treat disease before the onset of symptoms," says Garry Dolton, an immunologist at the Cardiff University School of Medicine.
"Early treatment is known to result in a better prognosis as the healthy pancreatic beta cells that are being attacked can be protected before they are destroyed," Dolton says.
"There is currently no cure for type 1 diabetes and patients require life-long treatment," Sewell notes.
"People living with type 1 diabetes may also develop medical complications later in life, so there is an urgent need to understand the underlying causes of the condition to help us find better treatments."
The study was published in The Journal of Clinical Investigation.
