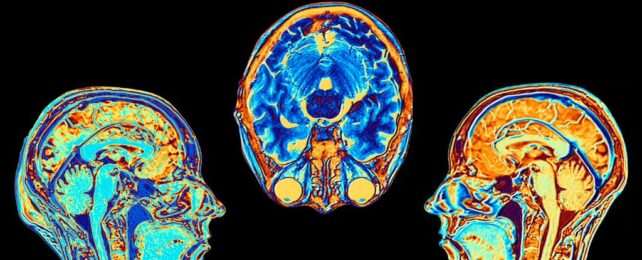
A gradual loss of brain tissue is a natural part of aging, but one of the longest-running brain scan studies has now revealed some people's neural connections deteriorate faster than others once they hit middle age.
According to a decades-long trial that began in 1995, those who show higher losses in white matter – the tissue that contains nerve fibers – have an 86 percent greater risk of developing mild cognitive impairment (MCI).
Compared to those without a metabolic disease, those with type 2 diabetes lost significantly more white matter over time, and this group ultimately faced a 41 percent higher risk of developing MCI.
What's more, people with biomarkers of dementia in their cerebrospinal fluid (CFS) had a nearly 50 percent higher risk of cognitive impairment.
If an individual had both diabetes and biomarkers of amyloid plaques (which are associated with Alzheimer's disease), that risk jumps to 55 percent.
Previous studies have also shown that significant losses in white matter are tied to cases of dementia, and that metabolic disorders can elevate a person's risk of cognitive decline.
But this is the first study to show a synergistic relationship between diabetes and amyloid plaques when it comes to their impact on white matter.
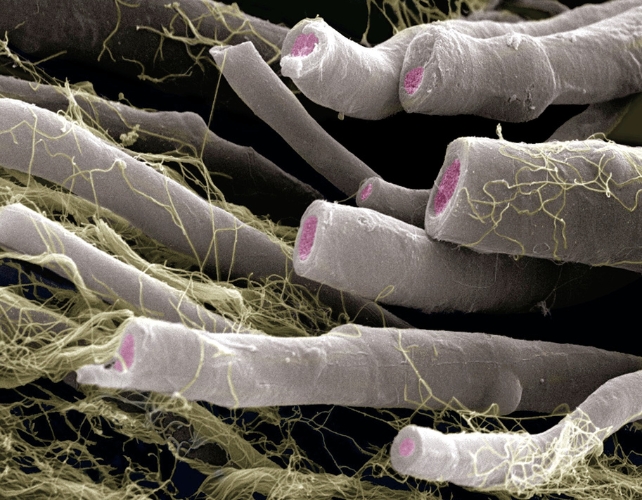
"These findings highlight that white matter volume changes are closely associated with cognitive function in aging, suggesting that white matter degeneration may play a crucial role in cognitive decline," write the authors of the study, led by neuroscientists at Johns Hopkins University in the United States.
"As insulin resistance plays a critical role in the formation of amyloid plaques, diabetes may promote Alzheimer's disease pathology, resulting in an earlier progression from normal cognition to MCI."
The long-term study was conducted among a group of 185 participants, who were mostly well-educated and White, with a family history of dementia.
It's not clear how well the findings will translate to more diverse populations, but most long-term MRI studies to date have been limited to less than a decade, and many only take two time points into account.
This newest study is impressively long, albeit small, tracking the brain shapes and sizes of participants at multiple points in their lives.
For up to 27 years, scientists regularly scanned the brains of participants, who started the trial with unimpaired cognition between the ages of 20 and 76.
At the end of the trial, 60 participants had progressed to mild cognitive impairment (MCI), and 8 of those participants went on to develop dementia.
Each person had their brain scanned about five times, and based on those images, it seems that it's normal as you age to gradually lose cortical gray matter, which contains neuron bodies, as well as white matter, which conducts messages between neurons.
What is unusual, however, is a more rapid deterioration in white matter, starting in middle age. Participants who experienced the greatest declines in white matter volumes, year to year, were far more likely to develop symptoms of MCI.
While only eight participants had a diagnosis of type 2 diabetes, the authors say their results suggest "that controlling diabetes may help reduce the risk of Alzheimer's dementia later in life as a modifiable risk factor."
Recent research, for instance, has shown that some drugs that treat type 2 diabetes are linked to a 35 percent lower risk of dementia in patients.
Physician-scientist Shohei Fujita, who was not involved in the study, reviewed the findings in an invited commentary for JAMA's Neurology.
Fujita applauds the "extended time frame" of the trial, and he hopes the findings "enable researchers and clinicians to develop targeted interventions for those most susceptible to progressive brain changes."
Notably, 63 percent of the cohort were women, and Fujita points out that "gender and race are also crucial variables that must be considered" in future longitudinal research.
After all, cognitive decline and dementia do not impact everyone in the same way. The way each individual brain shrinks with age is bound to be highly variable.
The study was published in JAMA Network.