A curious link between Alzheimer's and insulin resistance is now so well-established, the neurodegenerative disease is sometimes called type III diabetes.
Now a nasal spray developed by Italian researchers to exploit the link has delivered promising results stalling brain deterioration in mice modified to be at risk of a similar Alzheimer's-like condition.
Catholic University of Milan physiologist Francesca Natale and colleagues found an excess of a key enzyme in post-mortem brains of Alzheimer's patients called S-acyltransferase.
Previous research has revealed insulin resistance can influence the amount of these S-acyltransferase enzymes in the brain. The enzyme typically attaches fatty acid molecules to the infamously suspicious beta-amyloid and tau protein clumps, though in individuals with brain insulin resistance (BIR)-dependent deterioration the process can get out of control.
"In this new study, we showed that in the early stages of Alzheimer's molecular changes resembling a scenario of brain insulin resistance cause an increase of S-acyltransferase enzyme levels," says neuroscientist Salvatore Fusco, explaining how these enzymes then go on to alter cognitive function and the abnormal accumulations of protein clumps.
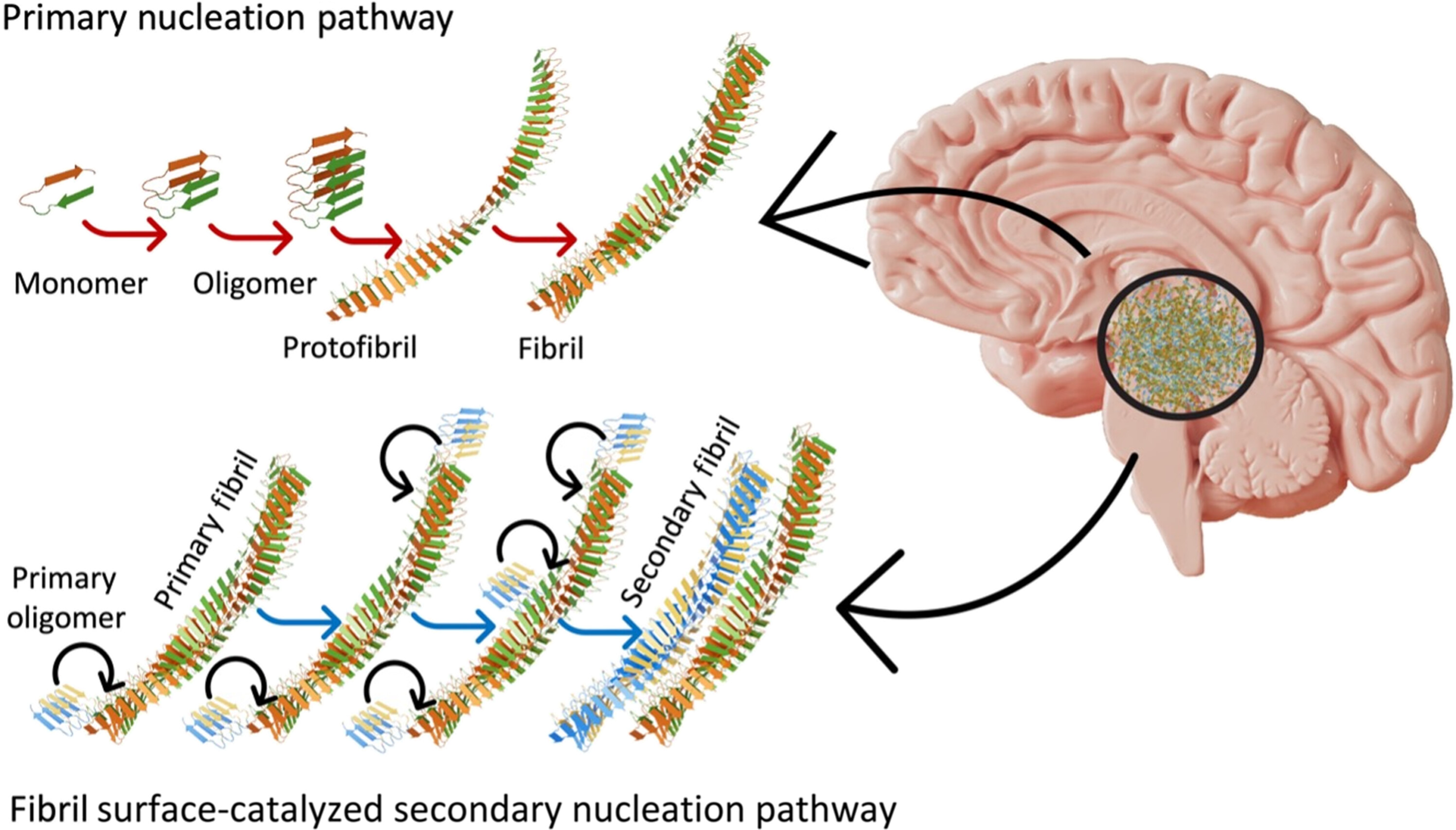
Beta-amyloid and tau are naturally occurring proteins that increase in Alzheimer's brains as the disease progresses.
Understandably, this has made the protein clumps a huge focus in Alzheimer's research. Yet, in a seeming contradiction, laboratory studies suggest the protein clumps do not directly damage brain cells. Treatments targeting these proteins have not been as successful as expected either, suggesting we're still missing crucial components of this disease.
So Natale and team disabled the function of the S-acyltransferase enzyme in mice genetically modified to have a mouse version of Alzheimer's disease.
Alzheimer's symptoms reduced whether the enzyme was turned off genetically or counteracted with an agent delivered through a nasal spray. Each treatment also seemed to slow the neurodegeneration and extend the rodent's lifespans.
The team did not detect any effects in normal mice given the same treatment.
The active agent in the nasal spray, 2-bromopalmitate, carries a high risk of interfering with a number of processes, making it unsafe for testing in humans. But the team is hopeful an alternative could be identified, now they have a specific target.
More studies will be needed before researchers can determine if this is a safe tactic. But with a new dementia diagnosis now being made every three seconds, and no cure, better treatments are urgently needed.
"New approaches – potentially translatable to human therapies – will be tested, including 'genetic patches' or engineered proteins that can interfere with [S-acyltransferase] enzyme activity," says neuroscientist Claudio Grassi.
The team's findings parallel another recent study that also suggests the problematic beta-alpha protein clumps can be both involved and somehow not involved in damaging brain tissues depending on the other molecules present with them.
"To date no therapeutic interventions targeting… [S-acyltransferase] have been attempted in Alzheimer's disease. Thus, our findings add a layer to the understanding of AD pathophysiology and identify potential therapeutic targets," Natale and team conclude.
This research was published in PNAS.
