Scientists are designing a new type of drug that mimics the physiological benefits of breathing in thin 'mountain air'.
Continuous low-oxygen, provided by a daily pill, could prove life-saving for people with serious metabolic diseases, like Leigh syndrome.
The new medicine, called HypoxyStat, extended the lifespan of mice with too much oxygen in their brains by up to 4-fold, reports a US team from Gladstone Institutes, the University of California San Francisco, and the pharmaceutical company Maze Therapeutics.
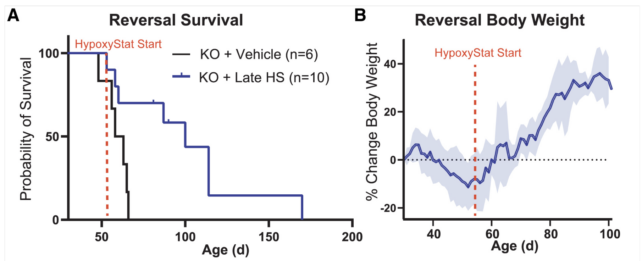
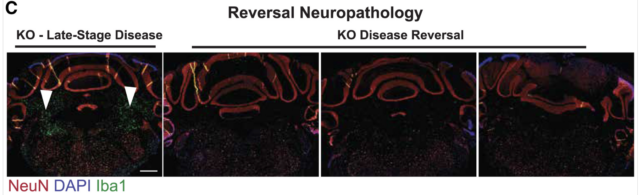
In their proof-of-concept experiment, the drug worked even when given to mice in a late stage of neurodegeneration, where brain lesions are extensive and some animals are on the brink of death. The advanced damage was reversed, and movement, muscle weakness, and loss of coordination were improved.
Leigh syndrome is a rare, progressive disease where mitochondria can't use the body's oxygen fast enough. Oxygen buildup in tissues can lead to damage and ultimately cell death. Children with Leigh syndrome often die within the first few years of life. Only about 20 percent make it to age 20.
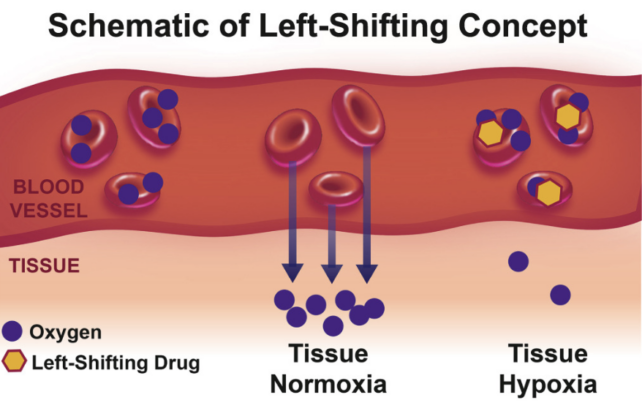
Typically, all but 2 percent of inhaled oxygen ends up in the body's mitochondria – famously known as the 'powerhouse' of the cell because of their ability to use oxygen for energy production. But in high-altitude regions, the body shifts so that oxygen is not as easily delivered from the bloodstream to tissues.
In a groundbreaking 2016 experiment, researchers found that for mouse models of Leigh syndrome, living in a low-oxygen environment not only prevents brain damage; it also reverses it. Further studies on mice in 2017 and 2019 confirmed those remarkable results.
It's not clear if humans with Leigh syndrome respond in the same way to low-oxygen environments. But biochemist Isha Jain from the University of California San Francisco (UCSF) and her colleagues are already exploring a way to mimic those effects pharmaceutically.
Unlike sleeping in a hypobaric chamber, as some athletes do when training for high-altitude events, a drug that tricks the body into functioning like it would high up in the mountains could work virtually all day, leaving a person free to go about their usual business, inside or outside.
"It's not practical for every patient with this disease to move to the mountains," says Jain, an author on all three of the papers as well as the current study.
"But this drug could be a controlled and safe way to apply the same benefits to patients."
Jain was previously a consultant for Maze Therapeutics, who sponsored this HypoxyStat study, and she has patents related to hypoxia therapy.
She and her colleagues hypothesized that by making red blood cells carry more oxygen in the bloodstream, as they do in high-altitude environments, the amount of oxygen offloaded into the body's tissues would be reduced.
In 2017, researchers found a drug, called GBT-440 or Voxelotor, that increases the affinity of the red cell protein hemoglobin to bind oxygen.
When Jain and her team, led by biochemist Skyler Blume, incubated human red blood cells with GBT-440, they noticed the cells increased their affinity for hemoglobin by 75 percent.
Emboldened by their results, the researchers found another compound like GBT-440 and named it HypoxyStat.
Mice with Leigh syndrome that were treated with HypoxyStat showed a significant reduction in brain damage, shown by the green markers of lesions in the image below.
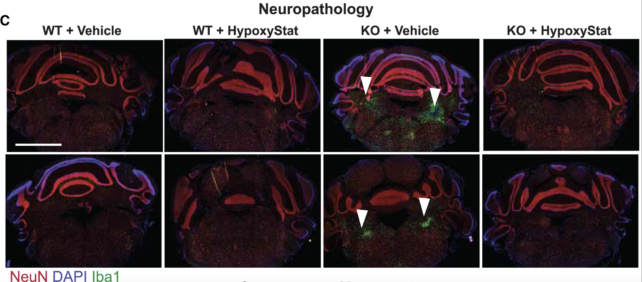
Even in later stages of the disease, a daily dose of this drug greatly extended mouse lifespans and reversed extensive damage in the brain.
"This ability to reverse advanced pathology positions HypoxyStat and related compounds as promising therapeutic candidates for mitochondrial diseases, where early diagnosis and intervention are often challenging," the authors of the study conclude.
The research team is now exploring a second-generation version of HypoxyStat that could better translate to primate models or human clinical trials.
"Gas-based therapies for disease are really unique, and being able to bottle them up into drugs is a new, unusual concept," says Jain. "We're excited to see where this promising strategy takes us."
The study was published in Cell.
