Researchers in the US have just made an existing chemotherapy drug way more effective, managing to kill drug-resistant lung cancer cells in the lab using 50 times less of the medication than is currently required.
"That matters because we may eventually be able to treat patients with smaller and more accurate doses of powerful chemotherapy drugs, resulting in more effective treatment with fewer and milder side effects," explained lead researcher Elena Batrakova, a pharmacologist at the University of North Carolina at Chapel Hill.
What's really exciting about the result is that it didn't rely on any new or experimental medications - the researchers were able to kill the drug-resistant cancer using chemotherapy that's already been tested and is known to work in humans - all they did was make it a whole lot better by figuring out a new way to package and deliver the medication.
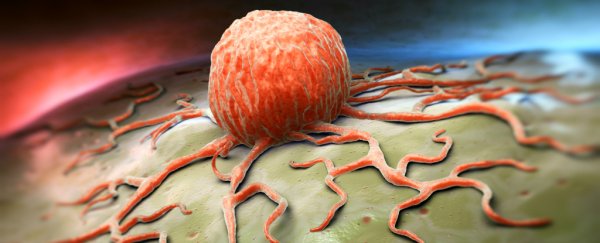
That's important, because chemotherapy is inherently inefficient. Basically it involves toxic medication being pumped into large areas of the body in the hopes of killing off cancer cells… which often works, but also happens to kill off a whole lot of other healthy tissue, resulting in some intense side effects.
For years, scientists have looked into better ways of targeting these drugs so that they only effect tumours and don't harm any other cells, but most of them have done this by using plastics-based nanoparticles to package the drugs. It's a good idea in theory, but the body usually recognises these nanoparticles as foreign and attacks, preventing the package from getting where it needs to be.
Instead, the North Carolina team looked for more natural alternatives, and packaged the drugs inside something called an exosome - tiny spheres harvested from a patient's own white blood cells.
"Exosomes are engineered by nature to be the perfect delivery vehicles," said Batrakova. "By using exosomes from white blood cells, we wrap the medicine in an invisibility cloak that hides it from the immune system. We don't know exactly how they do it, but the exosomes swarm the cancer cells, completely bypassing any drug resistance they may have and delivering their payload."
To test the system out, the researchers took a chemotherapy drug called paclitaxel, which is already used effectively to treat breast, lung, and pancreatic cancers, but with severe side effects, such as hair loss, muscle cramping, and diarrhoea.
The researchers loaded this drug inside exosomes taken from mice, and then set them loose on a petri dish containing multiple-drug-resistant cancer cells. They called their treatment exoPXT, and they found that they needed 50 times less of it to kill the cancer cells than they did when they used commercially available versions of paclitaxel.
The team also tested dye-filled exosomes in mice with drug-resistant lung cancer, and showed that the exosomes were able to thoroughly seek out and mark cancer cells, suggesting the little packages also have potential as highly accurate diagnostic tools.
The next step will be to see if the exosomes can deliver drugs just as well in these mice models and, if all goes to plan in the future, humans. But that's a big if - unfortunately, many therapies that are effective in the lab and even in mouse models don't end up working in humans.
Still, it's a pretty exciting first trial, and it suggests that exosomes could play an important role in the future of diagnosis, as well as treatment. We're looking forward to seeing what happens next.
The results have been published in Nanomedicine: Nanotechnology, Biology and Medicine.