Using the much-touted CRISPR/Cas9 gene editing method, scientists have demonstrated how they can edit HIV out of human immune cell DNA, and in doing so, can prevent the reinfection of unedited cells too.
If you haven't heard of the CRISPR/Cas9 gene-editing technique before, get ready to hear a whole lot more about it in 2016, because it's set to revolutionise how we investigate and treat the root causes of genetic disease. It allows scientists to narrow in on a specific gene, and cut-and-paste parts of the DNA to change its function.
CRISPR/Cas9 is what researchers in the UK have recently gotten approval to use on human embryos so they can figure out how to improve IVF success rates and reduce miscarriages, and it's what Chinese scientists were caught using in 2015 to tweak human embryos on the down-low.
Earlier this year, scientists started using CRISPR/Cas9 to successfully treat a genetic disease - Duchenne muscular dystrophy - in living mammals for the first time, and now it's showing real potential as a possible treatment for HIV in the future.
The technique works by guiding 'scissor-like' proteins to targeted sections of DNA within a cell, and then prompting them to alter or 'edit' them in some way. CRISPR refers to a specific repeating sequence of DNA extracted from a prokaryote - a single-celled organism such as bacteria - which pairs up with an RNA-guided enzyme called Cas9.
So basically, if you want to edit the DNA of a virus within a human cell, you need a bacterium to go in, encounter the virus, and produce a strand of RNA that's identical to the sequence of the virtual DNA.
This 'guide RNA' will then latch onto the Cas9 enzyme, and together they'll search for the matching virus. Once they locate it, the Cas9 gets to cutting and destroying it.
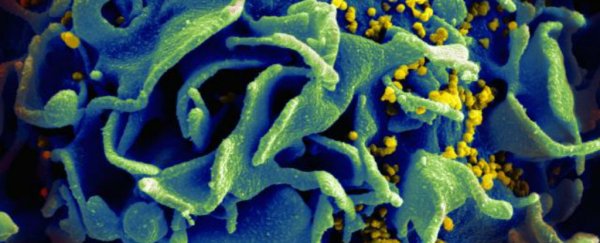
Using this technique, researchers from Temple University managed to eliminate HIV-1 DNA from T cell genomes in human lab cultures, and when these cells were later exposed to the virus, they were protected from reinfection.
"The findings are important on multiple levels," says lead researcher Kamel Khalili. "They demonstrate the effectiveness of our gene editing system in eliminating HIV from the DNA of CD4 T-cells and, by introducing mutations into the viral genome, permanently inactivating its replication."
"Further," he adds, "they show that the system can protect cells from reinfection and that the technology is safe for the cells, with no toxic effects."
While gene-editing techniques have been trialled before when it comes to HIV, this is the first time that scientists have figure out how to prevent further infections, which is crucial to the success of a treatment that offers better protection than our current antiretroviral drugs. Once you stop taking these drugs, the HIV starts overloading the T-cells again.
"Antiretroviral drugs are very good at controlling HIV infection," says Khalili. "But patients on antiretroviral therapy who stop taking the drugs suffer a rapid rebound in HIV replication."
There's still a lot more work to be done in getting this technique ready for something more advanced than human cells in a petri dish - particularly when it comes to perfect accuracy for the 'cutting' process - but it's an exciting first step.
The results have been published in Scientific Reports.