A type of bacteria that's resistant to the last antibiotic we have left against superbugs has made it to the US, and it signals something doctors have been dreading for years - the end for antibiotics.
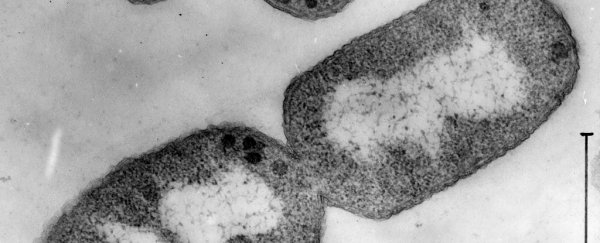
The bacterium, a strain of Escherichia coli, was found in the urine of a Pennsylvania woman. The strain is resistant to the antibiotic colistin, which doctors have been using as an absolute last-resort for bacteria that are extensively drug-resistant.
We've talked a lot about the problem with antibiotic resistance before, but in a nutshell, the reason why antibiotics are so important is because the easiest way to destroy bacteria is to douse them in alcohol or high heat, but that's not exactly something you really want to be doing when the bacteria are inside you.
Enter the gentler Plan B: antibiotics.
Antibiotics work by attacking a specific mechanism used by bacteria to function, but because bacteria are able to reproduce so quickly, natural selection has led to superbugs that have altered this mechanism and rendered the antibiotics useless.
And we're quickly running out of time to come up with new options - we've had antibiotics for about 85 years, and even in the first 10 years of use, bacteria were becoming resistant. In the 75 years since then, we haven't managed to create enough antibiotics to outrun the bacterial evolution.
And now, the one antibiotic we had left, colistin, is beginning to fail.
Bacteria that are resistant to colistin have been found before in Italy, China, and the UK, but this is the first time that the resistance has been found in the US. It's thought the resistance may have originated in Chinese pigs, because colistin has been used extensively in the pork industry.
colistin itself is a very old drug, and wasn't deemed useful until recently, because at certain doses it can be toxic to the kidneys. But because it was used so rarely, it meant that bacteria hadn't had a chance to build up resistance against it, which is why it's been so helpful against superbugs that nothing else could wipe out.
But, all good things must come to an end, and we could be back at square one.
While the strain of E. coli that the Pennsylvania woman had been infected with ended up being treated by other types of antibiotics - which is means it isn't resistant to everything, just colistin (yay!) – that doesn't mean it isn't dangerous.
As well as being able to pass genes on through reproduction, bacteria also have the ability to pass genes on laterally, which means between species or even different classes of bacteria. That means the particular gene that codes for colistin resistance, mcr-1, could spread to other types of bacteria in US that are already extensively resistant to antibiotics.
The worst news of all is that the diagnosed woman hadn't left the country in the last five months - so scientists have no idea how she got this resistant strain, and how many people around her might have been exposed.
"It basically shows us that the end of the road isn't very far away for antibiotics - that we may be in a situation where we have patients in our intensive-care units, or patients getting urinary tract infections for which we do not have antibiotics," said CDC Director Tom Frieden in an interview with The Washington Post.
Nearly 2 million American a year develop hospital-acquired infections, resulting in 99,000 deaths - the majority of which are caused by antibiotic-resistant pathogens. Without access to working antibiotics, routine surgeries will become dangerous, and a basic infection could be deadly.
Unfortunately, this issue is becoming closer to a reality every day. "The medicine cabinet is empty for some patients," Frieden said. "It is the end of the road unless we act urgently."
Researchers are now trying to find alternatives to antibiotics, such as microbe-killing copper hospital beds, and ancient remedies. Let's just hope they manage to come up with some solutions soon.
The case has been published in Antimicrobial Agents and Chemotherapy.