An international team of researchers has found evidence that the specific type of protein clumps in a person's brain might help identify different 'types' of Alzheimer's disease.
These findings might help future researchers and doctors accurately identify different subtypes of the disease, making treatments and diagnostic practices more specialised, pushing us one step closer to conquering Alzheimer's.
While you might not have heard of different 'types' of Alzheimer's before, researchers have previously found that the disease – which was once thought of as one single ailment – operates differently based on what subtype of the disease a person has.
In short, there are three known types of Alzheimer's: typical Alzheimer's, posterior cortical atrophy Alzheimer's, and rapidly progressive Alzheimer's.
"Because the presentation varies from person to person, there has been suspicion for years that Alzheimer's represents more than one illness," said Dale Bredesen, from the University of California, Los Angeles, who was not involved in the new study but did earlier work to identify the three subtypes.
"The important implications of this are that the optimal treatment may be different for each group, there may be different causes, and, for future clinical trials, it may be helpful to study specific groups separately."
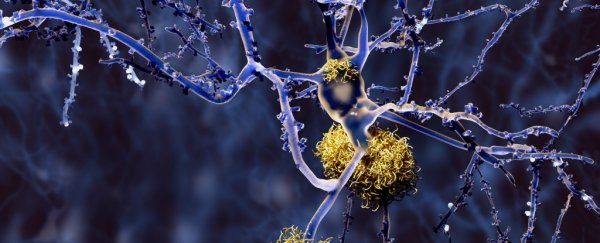
Earlier studies like the one Bredesen was involved with suggested that these subtypes might reveal themselves in how amyloid-beta peptides self-assemble into protein fibres known as fibrils in the brains of those with Alzheimer's.
Now, a team of researchers working with the National Institutes of Health (NIH) in the US and other agencies have found that these fibrils – which you can think of as 'protein clumps' – do, in fact, correlate with the different subtypes of the disease.
To come to that conclusion, the team – led by Robert Tycko, from the NIH – analysed the fibrils inside 37 different tissue samples from 18 individuals with each individual having one of the three subtypes of Alzheimer's.
When complete, the team found that the fibrils housed inside the tissue samples had a specific structure for those with typical Alzheimer's and posterior cortical atrophy, meaning that the presence of these structures could be a go-to indicator of these two types.
Those suffering from the rapidly progressive form of the disease, on the other hand, had a multitude of fibril structures, making it a lot harder to identify because there wasn't one specific structure belonging to it.
What these findings suggest is that doctors might be able to analyse tissue samples from patients who have been diagnosed with Alzheimer's to accurately judge which subtype of the disease they have.
That would mean they could then potentially administer a more suitable treatment for that specific type, offering new hope to those suffering from the disease.
Also, understanding how the three subtypes differ could lead to better, more specific treatments that can help us push forward to finding a cure for the disease in general.
"A better understanding of the neurotoxic amyloid-beta aggregates and of correlations between their structure and disease subtypes might help the development of new diagnostic tests and treatments for Alzheimer's disease," the team said.
It's important to note, though, that the sample size used for the recent study was quite small, with the team only analysing tissue from 18 individuals. It will take a more comprehensive pool of data before any conclusions can be drawn, though this is definitely a good first step.
In the US alone, about 5.4 million people suffer from Alzheimer's, costing individuals and families up to US$5,000 per year for care and costing the economy at large a whopping $236 billion per year. Finding a cure, or at least better treatments, is a major pursuit for scientists across the globe.
The team's work was published in Nature.