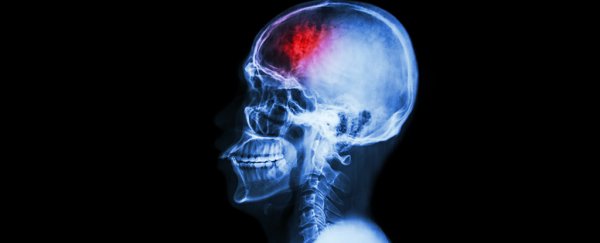
In yet another study that has connected conditions in the gut to diseases of the brain, scientists have linked the cause of common blood vessel abnormalities in the brain to bacteria colonies in the stomach.
These malformations can lead to strokes called cerebral cavernous malformations (CCMs), which don't leave patients with many options - if surgery can't be performed, there's little left but palliative care. But figuring out what causes these abnormalities could led to treatments that block them before they even occur.
An international team led by researchers from the University of Pennsylvania studied genetically engineered mice that were prone to developing vascular lesions in their brains.
Previous research had shown that inherited forms of the condition could be caused by mutations knocking out certain genes. These genes would normally suppress key signals affecting the growth of brain cells that made up the walls of the blood vessels.
While this discovery provides a way of identifying those at risk of developing a CCM, there are currently no drugs that replace the role of the missing genes, so not a lot can be done.
But since CCM varies significantly in individuals with these mutations, there is probably more to the story than just a few broken genes.
Enter the mouse studies
By studying the two populations of genetically engineered mice over a number of generations, the researchers discovered individuals that appeared to be resistant to developing the lesions, even though they still carried one of the CCM mutations.
Within this population of mostly resistant mice, a few pups continued to develop malformations. But, somewhat tellingly, these young mice also had abscesses in their abdomens caused by injections they had received during the research, hinting at a potential cause.
To test if these infections played a role in the development of CCM, 16 'resistant' mice were inoculated with a live species of gram negative bacterium called Bacteroides fragilis, which is normally found in the gut.
Of those, nine went on to develop vascular lesions and inflamed and abscessed spleens, suggesting that the bacteria had spread from the site of their infection to affect the growth of cells lining the brain's blood vessels.
Usually, gram negative bacteria such as B. fragilis affect the responses of cells in mammals such as humans and mice through a type of molecule on their outer membrane called a lipopolysaccharide (LPS), or endotoxin.
To see if it was this molecule specifically causing the malformation, the team injected the endotoxin from the bacteria into mice engineered with the mutated genes, as well as into normal, non-engineered mice.
As suspected, those with a broken gene that made them susceptible to CCM developed vascular lesions in their brain, while the mice with functional versions of the genes didn't.
The cells lining the blood vessels form what's called the blood brain barrier, which usually prevents toxic materials such as endotoxins and bacterial cells from getting into our central nervous system.
Just how the endotoxins are affecting these cells is something of a mystery.
"This still needs to be investigated," one of the team, Jaesung Peter Choi, from the University of Sydney in Australia, told ScienceAlert.
"However, we think CCM formation is driven by activation of immune receptors on the luminal, blood side of the blood-brain barrier."
When these immune receptors, called TLR4, are activated by an endotoxin, the cells of the blood brain barrier are encouraged to grow abnormally. The relevant genes would usually prevent this malformation, but in the mice with mutated versions, there's nothing to halt the process.
Importantly, differences in the TLR4 immune receptor in people could also account for some of the variations in the condition seen in people with CCM mutations.
Change a home, change a gut
Comparing CCM-susceptible mice raised in germ-free conditions with those raised in less sterile conditions demonstrated the bacteria in our environment play a key role in turning a mere mutation into a deadly disease.
While it's possible that therapies could be developed to target the TLR4 immune receptor, the researchers suggest focusing on the microbiome of the gut instead.
"Manipulation of gut microbiome-host interactions is a more exciting potential strategy to treat a life-long disease such as CCM," the team write in their report.
To test if they could use antibiotics to influence the development of lesions in mutated mice, the researchers bred several generations of mice while administering antibiotics to their mother, testing each generation for lesions and the number of bacteria in their gut.
Just as they'd found with their germ-free mice, a 96 percent drop in bacteria coincided with a similar decline in lesions.
Blasting our immune systems with antibiotics might not be a straight-forward solution, of course, and we also have to keep in mind potential differences between mice and humans.
We are also still learning just how complex our microbiota are, and the multitude of health conditions which are linked with the diversity of microorganisms in our digestive system.
Yet for a condition that currently has few treatments, doorways to new ways to prevent lesions in those who are already susceptible is no doubt a giant step forward.
This research has been published in Nature.