According to recent research, we're not entirely sure how many diseases the label ' diabetes' covers. But no matter what causes our bodies to struggle with their blood sugar levels, it's a serious condition that requires daily care.
Scientists have been working hard to find cures, new treatments, and better management techniques for the millions of people worldwide dealing with diabetes.
Here are some of the latest developments you need to know about.
1. Insulin producing implants made from stem cells
Clinical trials began last year for testing for ViaCyte's PEC-Direct device; a credit-card sized implant containing insulin-producing cells derived from stem cells.
Previous research had shown the implants could mature and function inside patients. Together with a cohort of volunteers who started testing in January, the new research should tell us soon whether the technology can help people with type-1 diabetes.
2. Brand new beta cells
Type 1 diabetes develops when a person's immune system wipes out insulin-producing beta cells in the pancreas.
But it turns out that another type of immature beta cell has been hiding in our pancreases all along, and scientists think it might be possible to use these 'virgin beta cells' to restore the functionality of the pancreas.
3. A common blood pressure medication
A drug on the World Health Organisation's list of essential drugs could have another purpose; blocking a molecule implemented in the autoimmune response that can give rise to type-1 diabetes.
Called methyldopa, the compound already has an important job treating high blood pressure in pregnant women and children. It's left to be seen if it could help reduce the incidence of diabetes in some way, but the fact it's already being used - rather than being stuck in the lab - makes for a promising find.
4. A unique transplant
One woman with severe type 1 diabetes has spent a year without insulin injections thanks to an experimental transplant.
Doctors implanted insulin-producing cells into a fatty membrane in the stomach cavity, and the success of the operation is paving the way towards more people receiving artificial pancreases.
5. An extreme diet
A clinical trial conducted on just 298 volunteers in the UK last year found an intensive weight management program could put type-2 diabetes into remission for those who lose a significant amount of weight.
The subjects were limited to roughly 850 calories a day for three to five months, consuming mostly soups and health shakes, before having more food introduced.
A similar study conducted on rats last year in the US also showed low calorie diets might help those who can stick to it reverse their condition.
6. Glucose-monitoring contact lenses
Until we can nail down a cure, there will always been a need to monitor those messy blood glucose levels.
Checking your tears for glucose using a smart contact lens, or monitoring your sweat with colour changing ink, could be a whole lot less invasive than drawing blood.
They're not new ideas, but constant improvements in miniaturising technology could mean these kinds of devices aren't too far off.
7. Loneliness could make us prone
While we can list a variety of genetic and lifestyle factors that affect a body's growing resistance to insulin, there's still a lot to learn.
A study published late last year involving nearly 3,000 subjects aged 40 to 75 found there seems to be a significant relationship between social isolation and type-2 diabetes.
It's not clear what the link might be, but having a few housemates or a local social group could make all the difference.
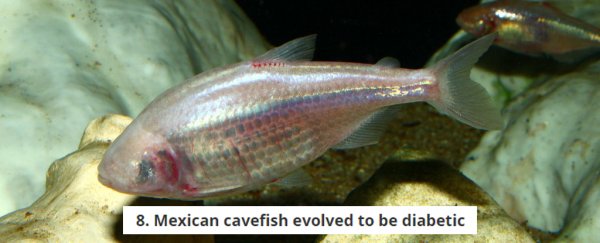
8. Mexican cavefish evolved to be diabetic
While developing a resistance to insulin is bad news in humans, the pale, eyeless animal known as a Mexican cavefish evolved a new version of the insulin receptor that makes it harder for the hormone to bind.
This isn't exactly a problem for the fish, which have also evolved other features to help it compensate. Studying its biology might help shine a light on how diabetes evolved in humans, and maybe even lead to new treatments.