Researchers have found intriguing evidence in mice that a blood-to-brain pathway could be responsible for introducing the toxic particles that contribute to Alzheimer's disease into our grey matter.
This work is still in very early phases, and we're a long way off being able to apply it to humans, but it's a compelling lead that could help us finally explain why the cause of the degenerative disease has proven so tricky to nail down and treat.
Decades of detective work have cast the protein fragment beta-amyloid as the top villain in the development of the dementia condition, Alzheimer's disease.
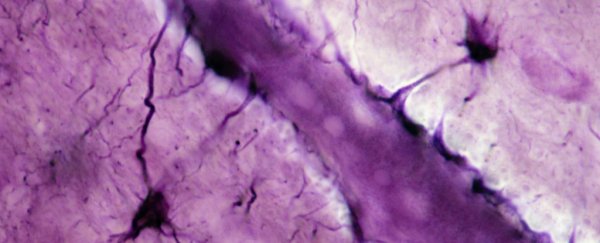
In spite of its reputation, there's still much we don't understand about this short chain of amino acids and its usual role in the body. What we do know is if it forms clumps in the brain, the long-term prognosis for mental health isn't a good one.
The case against beta-amyloid isn't exactly clear-cut, though.
Much has been discovered on its movement throughout the body and into the brain in recent years and how its presence eventually kills neurons. But nagging questions remain, such as why therapies targeting beta-amyloid plaques don't live up to expectations.
One ongoing area of interest is focusing not on the plaques but on the relationship beta-amyloid has with a class of fat-carrying chemicals called lipoproteins.
Using a transgenic mouse model, researchers from the Curtin Health Innovation Research Institute in Australia have uncovered compelling evidence that beta-amyloid proteins produced elsewhere in the body are smuggled into the brain via this lipid transport system.
"Our research shows that these toxic protein deposits that form in the brains of people living with Alzheimer's disease most likely leak into the brain from fat-carrying particles in blood, called lipoproteins," says lead investigator and physiologist John Mamo.
"This 'blood-to-brain pathway' is significant because if we can manage the levels in blood of lipoprotein-amyloid and prevent their leakage into the brain, this opens up potential new treatments to prevent Alzheimer's disease and slow memory loss."
The challenge for researchers has been to work out exactly how a small protein found throughout the body ends up accumulating in brain cells in such concentrations that it ultimately proves deadly.
One possibility is it is simply produced in large amounts right inside the brain's tissues. Yet having large concentrations of beta-amyloid in the peripheral blood is an exceptionally good predictor of developing brain plaques later.
One clue can be found in how a soluble version of low-density lipoproteins mops up about 70 to 90 percent of beta-amyloid in human plasma. There are also hints that leakage of this fat-carrying complex from capillaries deep inside Alzheimer's brains damages the blood vessels in signature ways.
Follow-up studies based on mice only further suggested there was some kind of link between lipoproteins and beta-amyloid. Rodents fed a diet rich in saturated fats (the kind they'd need plenty of lipoproteins for) presented the same leaky blood vessels in the brain, for instance.
Still, the possibility that the beta-amyloid could be generated inside the brain in toxic concentrations couldn't be ruled out as a contributing factor. So Mamo and his team engineered mice that could only express genes key to building beta-amyloid in their liver.
That way, any Alzheimer's-like pathology they could detect in the mice models' brains had to arise from beta-amyloid being carried in from the outside.
"As we predicted, the study found that mouse models producing lipoprotein-amyloid in the liver suffered inflammation in the brain, accelerated brain cell death, and memory loss," says Mamo.
Though there's plenty more work to be done, the discovery suggests there could be therapies for Alzheimer's disease that target the diet or use pharmaceuticals that manage how lipoproteins interact with beta-amyloid.
Aging populations around the globe can expect an increase in the number of people with Alzheimer's in the coming decades. Right now, more than 30 million individuals are thought to have the debilitating condition.
The more we can learn about the operations of beta-amyloid as it moves through our bodies, the better our chances of finding early ways to diagnose, treat, or even prevent the loss of neurological function that impacts so many lives.
This research was published in PLOS Biology.