Malaria still relentlessly plagues parts of the world. It killed more than 400,000 people in 2019, most of them babies and toddlers. In areas of Africa, it's even rivaling COVID-19 deaths, where the coronavirus pandemic has severely interrupted prevention and treatment efforts.
Now, to make matters worse, it looks as if a new strain of the primary parasite responsible for the disease, Plasmodium falciparum, is able to avoid a common way we detect it.
New research led by Ethiopian Public Health Institute's immunologist Sindew Feleke has shown nearly 10 percent of malaria cases are missed across Ethiopia's borders as a result of at least one of the mutations helping the parasite evade rapid diagnostic testing (RDT).
What's more, an ability to hide from test kits could easily give this mutated strain enough of an advantage to spread.
"False-negative results were common in multiple sites and will lead to misdiagnosis and malaria deaths without intervention," said University of North Carolina's infectious disease researcher Jonathan Parr. "This is a serious problem for malaria control efforts and a reminder that pathogens are very capable of adapting to survive."
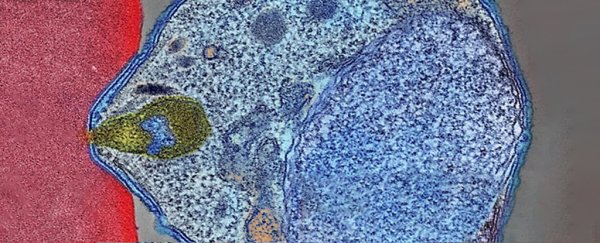
P. falciparum is the most common and deadliest of parasites responsible for malaria in humans. Spread by mosquitoes, the parasite infests human red blood cells to clone itself within. These blood cells eventually burst, sending floods of parasites into the bloodstream, causing waves of fevers and other nasty symptoms. Much of the disease's management revolves around reducing human contact with the blood-sucking insects.
Rapid diagnostic testing for malaria has helped Ethiopia – Africa's second-most populous country – make great strides against the disease in the last decade. With around 345 million sold annually, the most common rapid test detects antigens the parasite releases into the bloodstream. This is primarily histidine-rich protein 2 (HRP2), but the test can also be triggered by the closely related HRP3.
But some P. falciparum have mutations where the genetic instructions coding for the proteins (pfhrp2 and pfhrp23) have been deleted.
Studying the blood samples of over 12,500 patients along Ethiopia borders with Eritrea and Sudan, Feleke and team discovered these genetic variants had caused false-negative results for just under 10 percent of tests. This is double WHO's minimum criteria for triggering a change in national diagnostic strategy.
"We also found signs that RDT-based testing and treatment are driving a recent rise in pfhrp2 deletion mutation prevalence, allowing parasites to escape detection, " explained Parr.
While the mutations themselves were entirely random, this inadvertent selective treatment is allowing the parasites with either deletion in both the genes or sometimes just one gene or the other to flourish and spread.
The researchers mapped the sequences around the deletions for evidence of evolutionary pressure. This revealed pfhrp2 likely rapidly spread from a single, recent point of origin, with 30 of 31 strains forming a related cluster.
But pfhrp3 has been around longer, present in samples from 2013, and there are a number of different deletion patterns, suggesting it had multiple origins.
Unfortunately, other testing options are not as straightforward, and RDT that works by detecting other molecules produced by the parasite have not performed as well.
The team notes the way they picked up deletions in their study means they would have missed those who are asymptomatic, and they only sampled three sites, so they have not captured a complete picture of what these strains of malaria are doing yet. But evidence from Sudan, Djibouti, and Somalia suggest that the Horn of Africa may already be heavily infiltrated by the mutant P. falciparum.
"New tools are needed to support surveillance of [gene] deletions, determine their true prevalence and understand the forces impacting their evolution and spread," the team wrote in their paper.
The deletions are also present in South America, where RDT is not common. So they could be conferring some other evolutionary advantage, too, Feleke and colleagues suspect. It's possible that pfhrp2 does too. There is some evidence that pfhrp2 is involved in inflammation seen in severe malaria.
"People infected by pfhrp2/3-deleted parasites may have less severe disease and therefore be less likely to seek treatment, increasing the likelihood of onward transmission," explain the researchers.
But they can't yet rule out the possibility that its surrounding genes, also impacted by the deletion, are what's driving the parasite to become fitter. One of the flanking genes called EBL-1 is involved in P. falciparum's invasion of red blood cells.
"Surveillance across the Horn of Africa and alternative malaria diagnostic approaches in affected regions are urgently needed," said Parr.
This research was published in Nature Microbiology.