There's a hallmark of incurable neurodegenerative diseases – misfolded proteins that clump together to form sticky plaques or tangles called fibrils.
Now, new research has discovered that a protein normally tasked with clearing cells of molecular debris might be a common feature of a cluster of common and rare neurodegenerative diseases, including two distinct forms of dementia.
The finding was "both unexpected and surprising" and "raises many intriguing questions", according to the team behind the study, who made 3D-reconstructions of a twisted protein they found in "copious amounts" in some brain tissue samples.
"We have found that a protein called TMEM106B can form fibrils, and this behavior was not known before," says biophysicist and study author Xinyu Xiang of Stanford University.
The team extracted bulk proteins from brain tissue donated by 11 patients who had died from one of three neurodegenerative diseases: frontotemporal dementia, the most common form of dementia for people under age 60; progressive supranuclear palsy, a rare brain disorder which impairs balance, walking and vision; or dementia with Lewy bodies, a type of dementia often confused with Alzheimer's or Parkinson's disease.
"Each of these diseases has a unique protein tangle, or fibril, associated with it," says structural biologist Anthony Fitzpatrick of Columbia University. "These proteins associated with diseases have their own shapes and behaviors."
But in all 11 post-mortem brain samples, Fitzpatrick and colleagues found some previously undetected fibrils which, on closer inspection, appear to point "toward a commonality between these diverse neurodegenerative diseases."
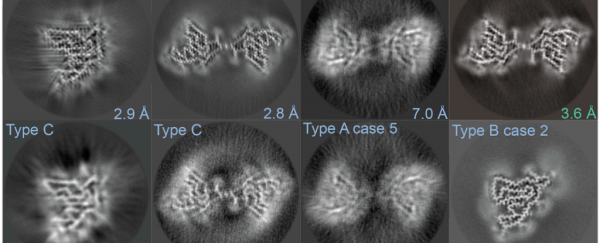
To investigate, the researchers used a technique called cryo-electron microscopy, or cryo-EM, which involves flash-freezing proteins to capture the fine details of their shape and structure, and is capable of resolving molecular features that are just 2 angstroms across – significantly smaller than a nanometer.
Fragments of the mysterious protein formed narrow twisted rods or stacked into wide, symmetric twisted ribbons, and this was most pronounced in the cases of frontotemporal dementia.
Based on these molecular structures, the researchers inferred the most probable sequence of the protein's amino-acid building blocks. When they scanned a database of known protein sequences, the fragments matched a protein that was actually identified more than a decade ago in a broad hunt for genes linked with frontotemporal dementia.
That protein is TMEM106B, which usually sits snug in the membranes of lysosomes and endosomes – two types of cell substructures (organelles) which gobble up cellular debris, malfunctioning proteins, and worn-out cell parts.
 Cryo-EM images of protein fibrils found in brain tissue samples (Chang et al., Cell, 2021)
Cryo-EM images of protein fibrils found in brain tissue samples (Chang et al., Cell, 2021)
The researchers speculate that the TMEM106B protein fragments and forms fibrils, which in turn disrupts lysosome function. This leads to a build-up of other known fibril-forming proteins, such as tau, which is implicated in Alzheimer's disease.
At this early stage, the microscopy data don't show that TMEM106B causes neurodegenerative disease, only that it happens to be present in the diseased brain tissue of a few people with different neurodegenerative diseases.
Also, finding that TMEM106B fibrils "occur across diverse proteinopathies makes it difficult to determine whether TMEM106B fibrils are disease-specific or are a general feature of neurodegeneration and aging," the team writes. They also note that another study, not yet peer-reviewed, recently found TMEM106B filaments in the brains of healthy older adults but not younger individuals.
What's more, Fitzpatrick and colleagues didn't detect these protein fibrils in their past studies of Alzheimer's disease and another brain disorder called corticobasal degeneration, so TMEM106B fibrils may not be a common feature across all neurodegenerative diseases, just some. It might also reflect the small number of samples analyzed thus far, from various brain regions.
Untangling what triggers the formation of TMEM106B fibrils, and if their presence amplifies or accelerates the accumulation of pathological proteins, as Fitzpatrick and colleagues suspect, could help to resolve some of these questions.
"We now have a promising new lead," says Fitzpatrick. "It could point towards a common thread linking a range of neurodegenerative diseases and could open the way to new interventions."
Bear in mind, however, that decades of research into therapies targeting the protein thought to be the main culprit in Alzheimer's disease, amyloid-beta, have led to many failed trials and much disappointment.
So, while there may be some commonalities between neurodegenerative diseases, their individual root causes remain elusive.
The study was published in Cell.