Scientists have identified the specific brain cells that die in Parkinson's disease and discovered what makes them so vulnerable.
Led by neurobiologists Tushar Kamath and Abdulraouf Abdulraouf of the Broad Institute, the team studied brain cells from individuals who had died from either Parkinson's disease or dementia, compared with people unaffected by either disorder.
What they found was a group of cells that were "highly susceptible" to degeneration, which could be prime candidates for therapeutic intervention. The study also shed light on how genetic risk likely manifests to produce Parkinson's disease.
Parkinson's disease is a progressive neurodegenerative disease characterized by uncontrollable movements such as tremors, speech difficulties, and balance problems that worsen over time. It is caused by damage to nerve cells that produce dopamine, a chemical messenger that regulates mood and body movements.
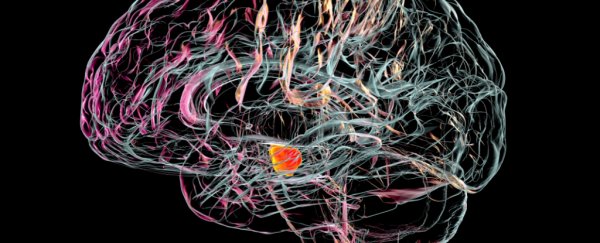
Loss of dopaminergic neurons in the part of the midbrain called the substantia nigra is a pathological hallmark of Parkinson's disease. While not all dopaminergic brain cells die, we do not yet have a firm grasp on the molecular features that make some neurons more vulnerable to disease than others.
The team of scientists behind this latest study set out to isolate and map thousands of individual neurons from the brains of people who had died from Parkinson's disease or dementia with Lewy bodies, a lesser-known form of dementia that can occur alone or together with other brain disorders.
Kamath and colleagues looked at roughly 22,000 brain cells isolated from human brain tissue samples of 10 individuals who died from either Parkinson's disease or dementia with Lewy bodies, and eight people unaffected by either disorder.
Measuring the levels of gene activity in single cells, the team identified 10 distinct subtypes of dopamine-producing neurons in the substantia nigra, each distinguishable by their gene activity profiles.
But one group of dopaminergic neurons stood out as largely missing in the brains of people with Parkinson's disease.
On closer inspection, they found that molecular processes linked to cell death in other neurodegenerative diseases were amped up in this particular group of dopaminergic neurons, and they pinpointed exactly where the cells usually reside: in the underside of the substantia nigra pars compacta.
What's more, this subset of neurons had the highest expression of genes that confer risk for developing Parkinson's disease, which might explain their unique vulnerability.
In other words, known genetic risk factors for Parkinson's disease might be acting upon "the most vulnerable neurons that influence their survival", Kamath and colleagues write in their paper.
It's important to note, however, that Parkinson's disease and dementia with Lewy bodies are two different disorders that share some similar features: midbrain dopaminergic neurons are lost, abnormal clumps of proteins called Lewy bodies form inside cells, and people often experience the same triad of motor movement impairments.
In light of these similarities, the new study "provides valuable information on common alterations in these two diseases," writes Ernest Arenas, a molecular neurobiologist at the Karolinska Institute, in a commentary accompanying the research.
However, some disease-specific alterations may be under-represented and undetected because of the small number of people sampled, he warns.
Nevertheless, now that we know more about the cells most vulnerable to Parkinson's disease and what makes them tick, researchers could engineer them in the lab by reprogramming skin cells – first into pliable stem cells, and then into the types of brain cells identified by Kamath and colleagues.
This painstaking process could allow scientists to probe the genetic drivers of the disease, screen potential drug candidates, or even explore the possibility of regenerative medicine for Parkinson's disease.
Integrating information from single-cell sequencing studies like this one with existing imaging data, tissue pathology studies, and genomic analyses would also help to refine our understanding of the defining features of Parkinson's disease, Arenas adds.
"This is a critical task, as our capacity to identify markers and actionable targets for [Parkinson's disease] will determine our capacity to develop novel therapeutics for this devastating disorder," he writes.
The study was published in Nature Neuroscience.