This might sound like the stuff of horror movies, but to treat some diseases you need to have drugs carefully injected into your eye.
Not only does the process sound terrible, there's actually quite a few things that could go wrong. For example, there's endophthalmitis – which is a bacterial infection caused by bacteria entering the hole where the needle went in.
You can also damage the eye tissue from repeated injection. Even worse, tumor cells could float through the newly made hole and spread to other areas.
With all that in mind, an international team of researchers have developed a new, potentially better system for delivering drugs to the eye without these complications.
The new technique has performed well in preclinical tests but unfortunately for our nightmares, it still involves eye needles.
"This novel improvement in drug delivery treatment can avoid problems associated with using needles to treat serious eye diseases," said one of the researchers, Terasaki Institute for Biomedical Innovation director Ali Khademhosseini.
The scientific term for injecting the eye is 'intravitreal injection', as it places the drug into the vitreous (jelly-like fluid that fills the eyeball). It's used to treat a number of diseases, including age related macular degeneration (AMD) and diabetic eye disease.
Currently, the treatment is multiple injections of a drug called anti-VEGF into the jelly-like substance in the eye.
So instead of having to rely on multiple infection-risking injections across treatments, the team created an ultrathin microneedle that actually stays in the eye and eventually biodegrades.
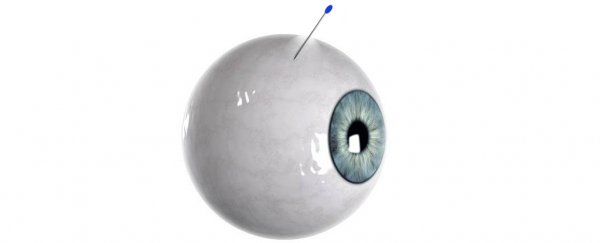
The microneedle has a hydrogel 'plug' to seal up the created hole and gradually releases the drug it is coated in while inside the eye area. You can see an illustration of what this looks like below.
 A graphical representation of the new design. (Lee et al., Advanced Healthcare Materials, 2022)
A graphical representation of the new design. (Lee et al., Advanced Healthcare Materials, 2022)
The researchers – who were mostly from institutions across South Korea – tested the new system in a couple of ways.
First, the team injected the microneedles into excised pigs eyes. This showed that the hole was sealed after the injection, and the drug (in this case a purple dye) spread through the eye as predicted.
Next, the team went a step further, inserting the microneedle into live pigs. The team found no leakage or inflammation at the site, and seven days later the tip of the needle was still securely lodged in place.
"It is also noteworthy that the fluorescent signal of [the model drug] rhodamine B was evident even in the deeper retinal tissues and retinal pigment epithelium at the farmost site from the tip of self-plugging microneedle," the team write in their new paper.
"These data indicate that [the model drug] from the tip of the self-plugging microneedle was successfully dispersed through the vitreous and the retina."
As usual with these kinds of experiments, there's a long way to go before you might be injected with a biodegradable self-plugging microneedle at your local optometrist. The design will need longer studies in animal models to ensure safety, and eventually undergo clinical trials to confirm if it's also safe in humans.
But for now, this is an exciting finding, and might provide a slightly less horrible solution to a very horrible problem.
The research has been published in Advanced Healthcare Materials.