"I just can't do what I used to anymore."
As pulmonologists and critical care doctors treating patients with lung disease, we have heard many of our patients recovering from COVID-19 tell us this even months after their initial diagnosis. Though they may have survived the most life-threatening phase of their illness, they have yet to return to their pre-COVID-19 baseline, struggling with activities ranging from strenuous exercise to doing laundry.
These lingering effects, called long COVID, have affected as many as one in five American adults diagnosed with COVID-19.
Long COVID includes a wide range of symptoms such as brain fog, fatigue, cough and shortness of breath.
These symptoms can result from damage to or malfunctioning of multiple organ systems, and understanding the causes of long COVID is a special research focus of the Biden-Harris administration.
Not all breathing problems are related to the lungs, but in many cases the lungs are affected.
Looking at the lungs' basic functions and how they can be affected by disease may help clarify what is on the horizon for some patients after a COVID-19 infection.
Normal lung function
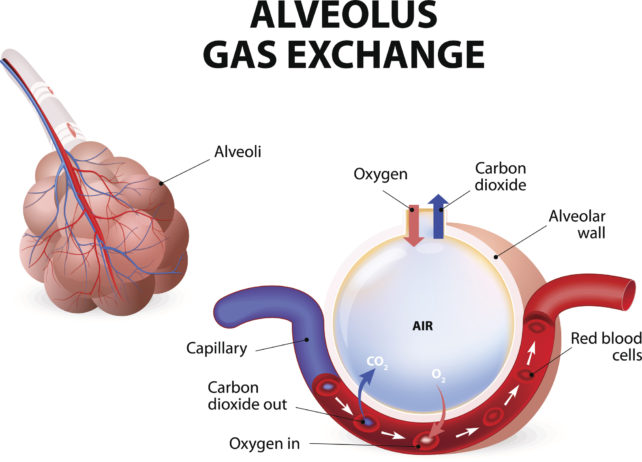
The main function of the lungs is to bring oxygen-rich air into the body and expel carbon dioxide. When air flows into the lungs, it is brought into close proximity with the blood, where oxygen diffuses into the body and carbon dioxide diffuses out.
This process, as simple as it sounds, requires an extraordinary coordination of air flow, or ventilation, and blood flow, or perfusion.
There are over 20 divisions in your airway, starting at the main windpipe, or the trachea, all the way out to the little balloons at the end of the airway, called alveoli, that are in close contact with your blood vessels.
By the time a molecule of oxygen gets down to the end of the airway, there are about 300 million of these little alveoli it could end up in, with a total surface area of over 1,000 square feet (100 square meters) where gas exchange occurs.
Matching ventilation and perfusion rates is critical for basic lung function, and damage anywhere along the airway can lead to difficulty breathing in a number of ways.
Obstruction – decreased airflow
One form of lung disease is obstruction of airflow in and out of the body.
Two common causes of impairments like these are chronic obstructive pulmonary disease and asthma.
In these diseases, the airways become narrowed because of either damage from smoking, as is common in COPD, or allergic inflammation, as is common in asthma. In either case, patients experience difficulty blowing air out of their lungs.
Researchers have observed ongoing airflow obstruction in some patients who have recovered from COVID-19.
This condition is typically treated with inhalers that deliver medications that open up the airways. Such treatments may also be helpful while recovering from COVID-19.
Restriction – reduced lung volume
Another form of lung disease is referred to as restriction, or difficulty expanding the lungs. Restriction decreases the volume of the lungs and, subsequently, the amount of air they can take in.
Restriction often results from the formation of scar tissue, also called fibrosis, in the lungs due to injury.
Fibrosis thickens the walls of the alveoli, which makes gas exchange with the blood more difficult.
This type of scarring can occur in chronic lung diseases, such as idiopathic pulmonary fibrosis, or as a result of severe lung damage in a condition called acute respiratory distress syndrome, or ARDS.
ARDS can be caused by injuries originating in the lungs, like pneumonia, or severe disease in other organs, like pancreatitis. Around 25 percent of patients who recover from ARDS go on to develop restrictive lung disease.
Researchers have also found that patients who have recovered from COVID-19, especially those who had severe disease, can later develop restrictive lung disease.
COVID-19 patients who require a ventilator may also have recovery rates similar to those who require a ventilator for other conditions. Long-term recovery of lung function in these patients is still unknown. Drugs treating fibrotic lung disease after COVID-19 are currently undergoing clinical trials.
Impaired perfusion – decreased blood flow
Finally, even when air flow and lung volume are unaffected, the lungs cannot complete their function if blood flow to the alveoli, where gas exchange occurs, is impaired.
COVID-19 is associated with an increased risk for blood clots. If blood clots travel to the lungs, they can cause a life-threatening pulmonary embolism that restricts blood flow to the lungs.
In the long term, blood clots can also cause chronic problems with blood flow to the lungs, a condition called chronic thromboembolic pulmonary hypertension, or CTEPH.
Only 0.5 percent to 3 percent of patients who develop a pulmonary embolism for reasons other than COVID-19 go on to develop this chronic problem.
However, there is evidence that severe COVID-19 infections can damage the blood vessels of the lung directly and impair blood flow during recovery.
What's next?
Lungs can work less optimally in these three general ways, and COVID-19 can lead to all of them. Researchers and clinicians are still figuring out ways to best treat the long-term lung damage seen in long COVID.
For clinicians, closely following up with patients who have recovered from COVID-19, particularly those with persistent symptoms, can lead to quicker diagnoses of long COVID.
Severe cases of COVID-19 are associated with higher rates of long COVID. Other risk factors for development of long COVID include preexisting Type 2 diabetes, presence of virus particles in the blood after the initial infection and certain types of abnormal immune function.
For researchers, long COVID is an opportunity to study the underlying mechanisms of how different types of lung-related conditions that result from COVID-19 infection develop.
Uncovering these mechanisms would allow researchers to develop targeted treatments to speed recovery and get more patients feeling and breathing like their pre- pandemic selves once again.
In the meantime, everyone can stay up to date on recommended vaccinations and use preventive measures such as good hand hygiene and masking when appropriate.![]()
Jeffrey M. Sturek, Assistant Professor of Medicine, University of Virginia and Alexandra Kadl, Assistant Professor of Medicine and Pharmacology, University of Virginia.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
