It's been 17 years since the coronavirus SARS-CoV threatened to erupt into a global pandemic. Thanks to rapid efforts to contain outbreaks of the infection, the world's population was spared the worst.
This time we weren't so fortunate. Just what makes SARS-CoV-2 so much more infectious than its predecessor is a question we're now a little closer to solving, with researchers uncovering yet another way the virus gains entry into our cells.
Researchers from the Technical University of Munich in Germany and the University of Helsinki in Finland led a study that discovered a receptor called neuropilin-1 gives the novel coronavirus a leg-up in infecting our tissues.
This particular protein is relatively abundant on cells lining the nasal cavity, making it a piece of cake for the virus to establish a home inside our bodies, raise a virus family, and then spread to a new host.
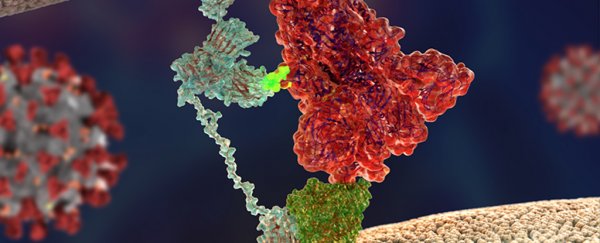
Earlier this year it was discovered that a receptor called angiotensin-converting enzyme 2 (ACE2) helps the coronavirus bind to the surface of cells, while an enzyme called Type II transmembrane serine protease (TMPRSS2) is crucial for it gaining entry.
This kind of molecular lock-picking does a good job of explaining why both SARS coronaviruses wreak havoc throughout a range of tissues in our bodies, from the lining of our lungs to our digestive tract.
But it doesn't say why one of the viruses does a better job of spreading than the other.
"The starting point of our study was the question why SARS-CoV, a coronavirus that led to a much smaller outbreak in 2003, and SARS-CoV-2, spread in such a different way even if they use the same main receptor ACE2", says University of Helsinki virologist Ravi Ojha.
A crucial piece of the puzzle appeared on comparing the two viral genomes; SARS-CoV-2 had picked up sequences responsible for producing a prickly array of 'hooks', not unlike those used by other nasty pathogens to grip onto host tissues.
"Compared to its older relative, the new coronavirus had acquired an 'extra piece' on its surface proteins, which is also found in the spikes of many devastating human viruses, including Ebola, HIV, and highly pathogenic strains of avian influenza, among others," says Olli Vapalahti, also a virologist from the University of Helsinki.
"We thought this could lead us to the answer. But how?"
Consulting with colleagues around the world, the researchers zeroed in on neuropilin-1 as a common factor.
Typically, this receptor plays a role in responding to growth factors important in tissue development, especially among nerves. But to many viruses, it's a convenient handle for holding onto host cells long enough to break in.
Electron microscopy of the surface spikes coating SARS-CoV-2 particles certainly hinted at the potential for a relationship with the receptor.
To help confirm it, the researchers made use of monoclonal antibodies specifically selected to block access to garden variety neuropilin-1, but not to mutant varieties tweaked to have a slightly different structure.
Sure enough, 'pseudoviruses' sporting SARS-CoV-2 proteins (great for watching viruses enter cells without worrying about the whole messy replication business that follows) had a much harder time getting inside when neuropilin-1 was locked up.
"If you think of ACE2 as a door lock to enter the cell, then neuropilin-1 could be a factor that directs the virus to the door," says Balistreri.
"ACE2 is expressed at very low levels in most cells. Thus, it is not easy for the virus to find doors to enter. Other factors such as neuropilin-1 might help the virus finding its door."
With neuropilin-1 expressed in large amounts in nerve tissues within the nasal cavity, we might imagine SARS-CoV-2 has a convenient red carpet rolled out for it the moment we sniff an infected droplet.
A close look at tissue samples expressing neuropilin-1 taken from deceased COVID-19 patients added to suspicions, while an experiment involving mice helped confirm the receptor's role in assisting the virus's entry into our nervous system.
Whether this might help explain why SARS-CoV-2 infections can have such a traumatic impact on the brain's function is a question for future research.
"We could determine that neuropilin-1, at least under the conditions of our experiments, promotes transport into the brain, but we cannot make any conclusion whether this is also true for SARS-CoV-2. It is very likely that this pathway is suppressed by the immune system in most patients," says neurologist Mika Simons from the Technical University of Munich.
It's tempting to picture new forms of antiviral medication on the horizon. Though as rapidly as SARS-CoV-2 reveals its criminal talents, simply blocking off cell receptors is likely to be bad news for our health.
That's not to say the discovery isn't without opportunity.
"Currently our laboratory is testing the effect of new molecules that we have specifically designed to interrupt the connection between the virus and neuropilin," says Balistreri.
"Preliminary results are very promising and we hope to obtain validations in vivo in the near future."
This research was published in Science.