New evidence from the US has backed up previous findings that as of early 2023, an estimated 6.9 percent of American adults – or some 17.8 million US citizens – have ever had long COVID.
The data reveal some clear demographic differences among US adults, showing which groups are more likely to be struck down for months or even years by the debilitating after-effects of COVID-19.
However, although the data captures the collective toll of long COVID in one country, which can crucially inform healthcare responses, lost in the numbers are the shattering experiences of individual long-haulers who are still fighting to have the chronic condition duly recognized.
For their sake, some researchers have been searching for mechanisms that might explain the lasting impact of long COVID and could lead to new therapies to root out the virus.
Others are trying to get solid answers to basic questions, such as how many people are affected by long COVID and what risk factors make someone more susceptible to the lingering and life-altering effects of an initial SARS-CoV-2 infection.
This new data comes from a nationally representative household survey of more than 17,400 US adults aged 18 years and over, analyzed by Zhengyi Fang and Rebecca Ahrnsbrak, two statisticians at the US Agency for Healthcare Research and Quality, which provides evidence to improve healthcare.
Of those surveyed, a total of 8,275 adults said they had been infected with SARS-CoV-2 at least once and 1,202 reported having had long COVID symptoms, such as flattening fatigue, brain fog, and difficulty breathing.
Across all age groups, females were more likely to report having had long COVID than males: 8.6 percent overall compared to 5.1 percent of males.
Younger people, who tend to be healthier, and older adults, who reported higher rates of booster shots, had lower rates of long COVID than middle-aged adults.
Rates of long COVID were also lower among vaccinated adults who had received a booster shot, compared to those who had received only two doses of a COVID-19 vaccine or were unvaccinated.
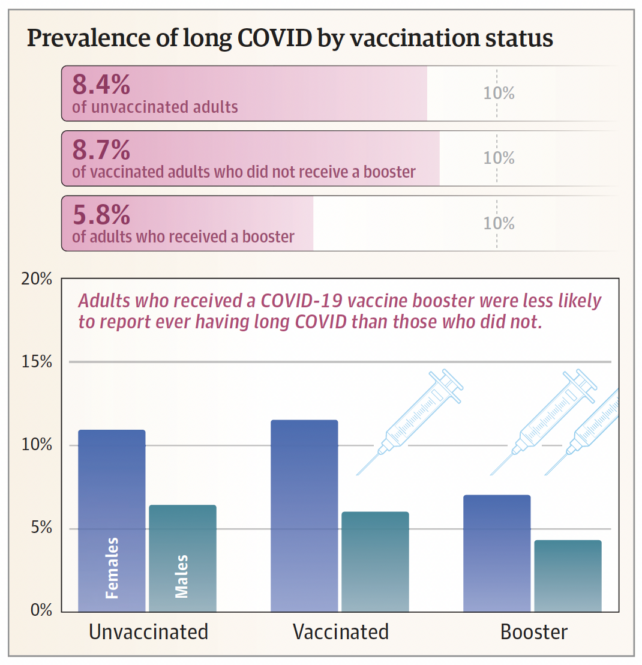
"These findings suggest that booster shots may enhance protection against long COVID, possibly because booster shots reduce the risk of severe COVID-19," Fang and Ahrnsbrak write.
Pre-existing chronic health conditions and obesity were flagged in the analysis as clear risk factors for long COVID, bolstering the findings from previous studies that also identified high blood pressure, depression, diabetes, and chronic obstructive pulmonary disease (COPD).
But as for overall prevalence, it depends on how long COVID is defined, based on how long symptoms persist (in this study, it was 3 months) and which symptoms are counted.
This is complicated by the fact people can experience a whole constellation of symptoms that don't always necessarily register on medical tests.
Country to country and over time, estimates of long COVID have varied, affected by different viral variants circulating throughout the pandemic and vaccination rates.
In Scotland, a nationwide study found 6.5–10 percent of adults had long COVID 6–18 months after infection, while 5–10 percent of Australian adults reported persistent symptoms 3 months after testing positive. In the Netherlands, rates were slightly higher, with one in eight people (or 12.7 percent) having had long COVID as of August 2022.
From studies like these, it's been estimated that 65 million people worldwide have developed long COVID, taken as 10 percent of the more than 651 million people who have had COVID-19 as of 2022.
Researchers have questioned those crude global estimates though, based on how they were calculated, extrapolating from national studies. Others argue we are likely underestimating the collective toll of long COVID, given the untold number of cases not documented in health records or surveys.
As that academic debate rolls on, COVID-19 case numbers continue to rise and fall. And although the severity of acute illness may be eased by available treatments, the burden of long COVID remains for long-haulers who tread the underworld.
The data brief has been published in JAMA.
