Immune cells in the blood of people with Alzheimer's disease exhibit subtle changes to how their genes are read, which could be a way the body primes itself to fight this insidious neurodegenerative disorder.
Researchers from Northwestern University in the US found sections of DNA in the peripheral immune cells of Alzheimer's patients unwind in a specific way, exposing genes that could help mount a response inside the brain.
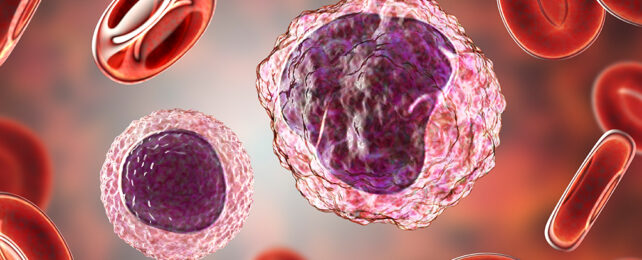
While much research has focused on the immune system operating within or near the brain in patients with Alzheimer's, surprisingly little has been devoted to investigating potential differences in white blood cells throughout the rest of the body.
"It is possible that these findings implicate the peripheral immune response in Alzheimer's disease risk," says neurologist David Gate. "We haven't yet untangled whether these changes are reflective of brain pathology or whether they precipitate the disease."
Alzheimer's disease is a progressive degeneration of brain tissue, typically in areas critical to memory.
Though numerous genes have been implicated and pathologies are common among individuals diagnosed with the illness, researchers have yet to pinpoint what triggers the cascade of effects responsible for the damage, which may vary between individuals.
With the focus increasingly turning to changes outside of the nervous system, Gate and his team of researchers used single-cell gene translation technology to analyze individual white cells taken from 26 healthy participants and 30 who qualified as having Alzheimer's disease.
Different white cells perform distinct tasks in an immune response, whether it's the production or preservation of antibodies or the active destruction of potentially dangerous interlopers and invaders.
Every type of white cell in Alzheimer's patients investigated was found to harbor epigenetic changes – tweaks in DNA chemistry that enhance or interfere with the expression of one or more genes. In this instance, the changes exposed sequences within the cell's chromosomes, allowing them to be read more easily.
Looking closer at the kinds of genes being exposed, the researchers identified traits that could reasonably allow the cells to engage with Alzheimer's pathology in some way.
For example, large white cells called monocytes were found to have changes dependent on the kind of apolipoprotein E genotype they possessed, a combination of genes that can affect an individual's risk of developing Alzheimer's.
Curiously, a type of white blood called a CD8 T cell presented a little differently in people with the condition. Thanks to key epigenetic changes, a membrane protein called CXC motif chemokine receptor 3 (CXCR3) on these T cells stands out more clearly in those with Alzheimer's and guides the cells to the brain.
Why T cells might function this way isn't clear, though the fact the immune cells are typically kept out of the brain, lest they cause trouble, provides a few clues.
"The brain is emitting a signal that it is damaged, and the T cells are homing to that signal by their antenna, CXCR," says Gate.
"T cells can be very toxic in the brain, but we also don't know if these cells might be attempting to repair the damage in the brain."
How and why these epigenetic changes emerge is a topic for future research. Yet knowing they exist could lead to deeper insights into how the condition progresses, or even provide new therapeutic targets.
This research was published in Neuron.