As COVID-19 relentlessly infects more and more of us, scientists are getting a close look at the strange and frightening damage it can inflict on our bodies.
We've known since early in the pandemic this disease wreaks havoc on more than just the respiratory system, also causing gastrointestinal conditions, heart damage and blood clotting disorders.
Now, a year into the pandemic, in-depth autopsies of COVID-19 patients have revealed greater details of widespread inflammation and damage in brain tissues. This may help explain the deluge of neurological symptoms that have manifested in some patients, from headaches, memory loss, dizziness, weakness and hallucinations to more severe seizures and strokes.
Some estimate that up to 50 percent of those hospitalised with COVID-19 could have neurological symptoms that can leave people struggling to do even common daily tasks like preparing a meal.
"We were completely surprised. Originally, we expected to see damage that is caused by a lack of oxygen," said physician and clinical director at National Institute of Health (NIH), Avindra Nath.
"Instead, we saw multifocal areas of damage that is usually associated with strokes and neuroinflammatory diseases."
The NIH researchers, including physician Myoung-Hwa Lee and Nath, performed close examinations of brain tissues from 19 deceased patients. They ranged from 5 to 73 years old and many had risk factors for severe coronavirus, including diabetes and cardiovascular disease.
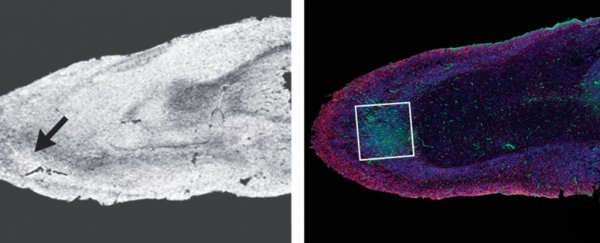
Using powerful MRI microscopy, Lee and team identified 10 patients with brain abnormalities. Closer examination under a microscope revealed hyperintensities - bright spots in the micrograph image of the brain samples - which fluorescent microscopy showed to be leaked fibrinogen (a blood protein).
T cells and the brain's specialised immune cells, microglia, surrounded these spots in a number of patients; there were also dark areas of clotted bleeding. These led the researchers to conclude these patients had experienced multiple, mini brain bleeds - a type of damage usually associated with inflammation in the brain.
"The very small blood vessels in the brain were leaking," Nath told NPR. "And it wasn't evenly - you would find a small blood vessel here and a small blood vessel there."
It's not just those seriously ill enough to require intensive care, or have pre-existing conditions, that have displayed neurological symptoms from COVID-19.
"We've seen this group of younger people without conventional risk factors who are having strokes, and patients having acute changes in mental status that are not otherwise explained," University of Liverpool neurologist Benedict Michael told Nature back in September.
Patients have suffered delusions and developed psychosis. In one case, a 55-year-old woman started seeing lions and monkeys in her home, before believing a friend or family member had been replaced by an identical imposter (a Capgras delusion).
Despite tests to detect the virus in the brain tissues, Lee and team found no trace of SARS-CoV-2, but caution in their report: "It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays."
While other studies have located traces of the virus in the brain, the levels were low and appear to be rare.
"So far, our results suggest that the damage we saw may not have been caused by the SARS-CoV-2 virus directly infecting the brain," said Nath. Instead the damage may be due to the body's inflammatory response to the virus, he explained.
Because of low sample size and limited clinical information the team says they can't draw any direct conclusions just yet. But their findings align with EEG tests that have revealed encephalopathy in COVID-19 patients - disturbances in the brain's typical electrical activity that can signify swelling and inflammation.
It also aligns with studies showing the virus can trigger other dangerous immune responses that in some cases cause even more harm than the virus itself has directly.
Researchers are concerned about the implications of brain inflammation on people's long-term health, given it's associated with memory loss and Alzheimer's disease and some patients are already suffering lingering neurological consequences such as chronic fatigue and Guillain–Barré Syndromes.
"In the future, we plan to study how COVID-19 harms the brain's blood vessels and whether that produces some of the short- and long-term symptoms we see in patients," said Nath.
Their report was published in the New England Journal of Medicine.