Antibiotic resistance, one of the biggest health threats of our time, has been spreading its wings across the face of our planet. And now, researchers have detected signs of it in one of the most remote inhabited areas on Earth.
In an effort to discover more about what drives the spread of antibiotic resistance, researchers turned to soil samples in Svalbard, an archipelago in Norway up in the High Arctic close to the North Pole.
Here, the team detected more than you'd ever expect from such a far location - traces of 131 different antibiotic-resistant genes (ARGs) responsible for the spread of superbugs. These include the blaNDM-1 gene, first detected in urban India around 8,000 kilometres (or 5,000 miles) away from Svalbard.
Scientists think this particular gene was possibly carried by faeces of migratory birds, other wildlife, and even human beings.
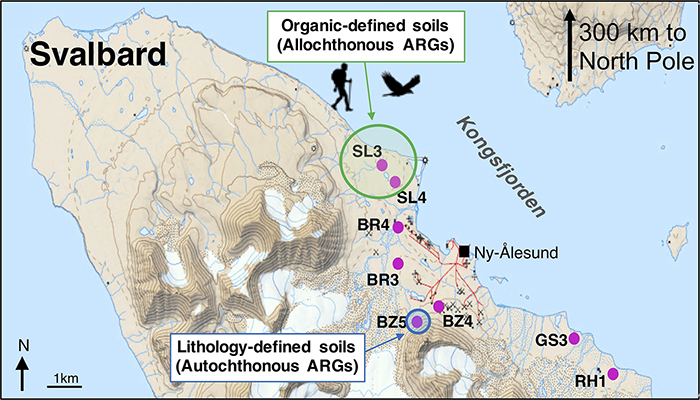
The team chose the Kongsfjorden region of Svalbard as their study site because it's on a remote island with no agriculture or industry, and it's so cold here all year round that it's easy for DNA to be preserved in the soil. On top of that, less than 120 people live in this frigid patch of land at any one time.
The wanderlust of blaNDM-1 to a spot far away from large hospitals and urban civilisation is another sign that tackling antibiotic resistance (AR) is a global rather than a local challenge.
 (Environment International)
(Environment International)
"Polar regions are among the last presumed pristine ecosystems on Earth, providing a platform for characterising pre-antibiotic era background resistance against which we could understand rates of progression of AR pollution," says one of the researchers, environmental engineer David Graham from Newcastle University in the UK.
"But less than three years after the first detection of the blaNDM-1 gene in the surface waters of urban India we are finding them thousands of miles away in an area where there has been minimal human impact."
We know that by coding an enzyme called NDM-1, the blaNDM-1 gene can help to develop resistance to multiple drugs in microorganisms – even "last resort" drugs like carbapenems, the ones that we try when all else has failed.
And as bacteria evolve to fight the best treatments we can throw at them – evolving from plain old ordinary bugs to superbugs – it's already costing thousands of lives every year, according to some estimates.
That situation will only get worse unless we can find ways to make our antibiotics more effective, or develop new varieties of them.
"Through the overuse of antibiotics, faecal releases and contamination of drinking water, we have consequentially speeded-up the rate at which superbugs might evolve," says Graham.
"For example, when a new drug is developed, natural bacteria can rapidly adapt and can become resistant; therefore very few new drugs are in the pipeline because it simply isn't cost-effective to make them."
While there's no immediate health threat to the area, antibiotic overuse in a clinical setting can't have led to the arrival of blaNDM-1 in such a remote region, which is why scientists are exploring other possibilities.
DNA was extracted from forty different soil core samples taken across the region of Kongsfjorden in 2013. The 131 resistance genes detected covered nine different antibiotic classes, with blaNDM-1 found in 60 percent of the cores.
The researchers describe soil as "both the source and sink" of antibiotic resistance, and are hoping to use Arctic soils as a baseline for measuring resistance and its spread – something that's going to be difficult with human-driven microbial movement.
There's still hope for finding and sampling more pristine, ARG-free soil in these regions. By doing that, scientists are aiming to better understand how antibiotic resistance develops and grows, and from there figure out better ways to stop it.
For that to happen, the team suggests, we need to take a long hard look at waste management, water quality, and other human impacts in the environment to keep the Arctic environment as pristine as it often looks.
"Encroachment into areas like the Arctic reinforces how rapid and far-reaching the spread of antibiotic resistance has become, confirming solutions to AR must be viewed in global rather than just local terms," says Graham.
The research has been published in Environment International.
