Scientists have identified five distinct biological variants of Alzheimer's disease, which appear to differ in how they affect the brain and, potentially, how they respond to treatment.
The international research team that analyzed cerebrospinal fluid proteins in 606 people says this means that medications already tested may have falsely seemed to be ineffective or only slightly effective.
Their discovery could lead to more personalized therapies or preventive measures for these subtypes. It also presents hope for early diagnosis and intervention to delay the onset of symptoms of Alzheimer's disease (AD).
"Given the distinct patterns of molecular processes and AD genetic risk profiles, it is likely that AD subtypes will require specific treatments," write neuroscientist Betty Tijms from Alzheimer Center Amsterdam and colleagues.
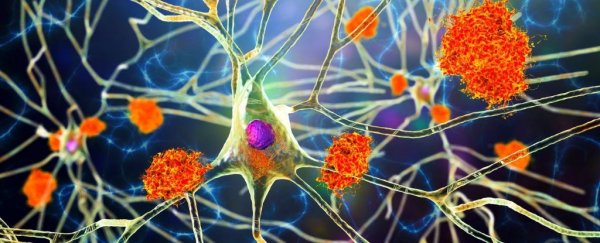
Alzheimer's disease – a neurodegenerative disorder that affects millions of people worldwide – is characterized by the buildup of amyloid and tau proteins in the brain, leading to progressive memory loss and cognitive decline.
In addition to the buildup of amyloid and tau proteins forming clumps and tangles inside brain tissue, we know other biological processes in other tissues are involved. Using updated technology, researchers were able to accurately measure critical components of these other processes.
Tijms and her team used mass spectrometry proteomics to analyze cerebrospinal fluid from 419 people with Alzheimer's and 187 controls, looking for differences in protein levels. This led to the selection of 1,058 Alzheimer's-related proteins for analyses.
The researchers were able to identify five distinct biological subtypes of the disease, distinguished by variations such as hyperplasticity, immune activation, RNA dysregulation, choroid plexus dysfunction, and blood-brain barrier impairment.
Each variation was characterized by specific alterations in clusters of proteins related to inflammation, nerve cell growth, and other biological processes.
"Three subtypes recapitulated our previously identified three subtypes (hyperplasticity, innate immune activation and blood–brain barrier dysfunction)," Tijms and team explain.
"We further identified two additional AD subtypes: one with RNA dysregulation and one with choroid plexus dysfunction."
Identifying each variant's biomarkers may help us diagnose Alzheimer's earlier, when intervention is most effective.
The researchers also looked at magnetic resonance imaging ( MRI) scans from a subset of 503 participants to compare subtypes to individual volume differences in certain brain regions.
"Subtypes had distinct AD genetic risk profiles," the team writes, adding that they "also differed in clinical outcomes, survival times, and anatomical patterns of brain atrophy."
Hyperplasticity seems to involve an overactive cellular growth response, leading to amyloid and tau protein buildup.
In innate immune activation, the immune system goes into overdrive, excessively attacking healthy brain tissue.
RNA dysregulation involves changes in the transport of proteins along axons that allow nerve cells to function correctly.
Choroid plexus dysfunction impacts the ventricular system of the brain, which contributes to cerebrospinal fluid production and transfer of nutrients to the brain.
Blood-brain barrier impairment weakens the barrier protecting the brain, allowing damaging molecules to infiltrate. Unlike hyperplasticity, this subtype features slow nerve cell growth and low amyloid production.
This could mean some drugs only work in one Alzheimer's type. Amyloid focused medication, for instance, may treat a subtype with increased amyloid production but potentially harm a subtype with decreased production.
"Side effects arising from certain treatments may also depend on subtype," the authors say. "For example, while antibodies may more easily cross the blood–brain barrier in subtype 5, these individuals may be at increased risk for cerebral bleeding that can occur with antibody treatment."
Traditionally, Alzheimer's has been viewed as a single disease with some variations in symptoms and progression. Despite extensive research, there's no cure, and current treatments only offer limited symptom management.
More studies are needed to validate these new findings, and investigate whether variants do respond differently to medicines.
That said, this is an exciting step forward in the ongoing fight against Alzheimer's, and each discovery like this brings us closer to finding a cure.
The research has been published in Nature Aging.