More than 1,000 people die each day from asthma, a condition that restricts the airway and prevents sufficient oxygen from getting where it's needed.
In addition to an asthma attack's tightening of the channels into the lungs, inflammation of the lining and increased mucus production exacerbate the problem for weeks or months at a time, putting people at risk of triggering ongoing episodes.
Scientists have now shown for the first time how mechanical constriction of the airways during an asthma attack overcrowds cells in the lining. These cells are squeezed out and killed, which triggers inflammation, mucus secretion, and airway barrier damage.
"Without this barrier, asthma sufferers are far more likely to get long-term inflammation, wound healing, and infections that cause more attacks," says cell biologist Jody Rosenblatt from King's College London, senior author of the new study.
"By understanding this fundamental mechanism, we are now in a better position to prevent all these events. Our discovery is the culmination of more than ten years' work."
And they have a promising solution: a compound that blocks this squeezing out of overcrowded cells – called epithelial extrusion – in the airway lining of mice. Though its safety has yet to be tested in humans, Rosenblatt and her colleagues from the US, UK, and Spain think this could lead to entirely new approaches to preventing asthma attacks, not just treating inflammation.
Asthma affects around 300 million people worldwide. Most experience wheezing, coughing, shortness of breath, and chest tightness. Everything from pollen and dust mites to pet dander and smoke to exercise and even cold air can set off these symptoms, which range in severity.
No cure exists, but some treatments, particularly those that target airway inflammation, can control asthma symptoms. Inhaled bronchodilators to open up airways and corticosteroids to reduce inflammation are often used.
Avoiding triggers can help too, though even a combined approach isn't always effective.
"We know that around 31 percent of people with asthma don't have treatment options that work for them, putting them at risk of potentially life-threatening asthma attacks," says Samantha Walker, director of research and innovation at Asthma + Lung UK, who wasn't involved in the study.
The team studied bronchoconstriction, which is the tightening and squeezing of the smooth muscle around the airways during an attack. Constricting airways in mice caused lung lining damage and inflammation, like that seen in asthma.
"This constriction and destruction of the airways causes the post-attack inflammation and excess mucus secretion that makes it difficult for people with asthma to breathe," says Rosenblatt.
Albuterol is thought to be the best bronchodilator treatment, and in analysis of mice and human airway tissue, the researchers found it relaxes surrounding smooth muscle. But it doesn't stop airway epithelial cell damage, or the inflammation that comes after an asthma attack.
"Fortunately, we found that we can use an inexpensive compound, gadolinium which is frequently used for MRI imaging, to stop the airway damage in mice models as well as the ensuing inflammation and mucus secretion," Rosenblatt explains.
"Preventing this damage could then prevent the build-up of musculature that cause future attacks."
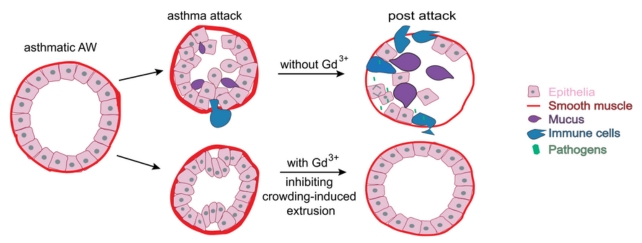
In a previous study, Rosenblatt and another team had found that gadolinium (Gd3+) blocks extrusion. This research demonstrated that it could stop extrusion in mice in a more clinically relevant way, after bronchoconstriction started. Gd3+ seemed to allow the lining of the airways to reattach to the surrounding smooth muscle as the albuterol helped it to relax.
Even if Gd3+ isn't found to be safe for treatments in humans, scientists may yet be able to develop similar therapies that target the extrusion pathway to prevent symptoms.
"This discovery opens important new doors to explore possible new treatment options desperately needed for people with asthma rather than focusing solely on inflammation," Walker says.
The authors suggest a similar mechanism could underlie other inflammatory conditions characterized by constriction, such as irritable bowel syndrome or inflammatory bowel disease. Clearing up the mystery around how these occur could lead to much needed treatments.
The research has been published in Science.
