A widely-used cancer drug that works on the immune system could push HIV out of hiding, potentially leaving the virus open to being attacked and eliminated, according to promising results from a small new study.
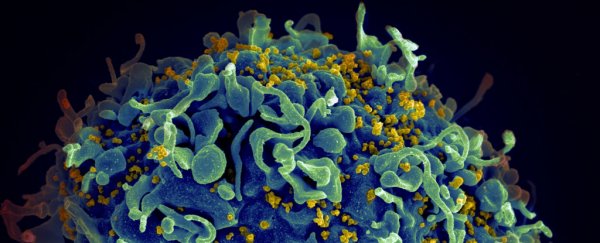
HIV (human immunodeficiency virus) almost needs no introduction: the virus is notorious for its ability to evade the immune system. Key to its insidiousness is viral latency – HIV 'hides' inside long-lived immune cells, inserting its genetic material into the cell's own, so it can escape detection.
This has been a major barrier to developing a cure for HIV, as the virus is never eradicated entirely with antiviral therapies, but continues to be present in the body within these latent reservoirs.
The new study suggests that pembrolizumab, an immunotherapy drug which has transformed the treatment of melanoma and other cancers, might also be able to reverse HIV latency, flushing the virus out of hiding.
Although the trial was only small, featuring 32 people living with both HIV and cancer, it is the largest study of its kind to date and the results are "very exciting", says infectious disease expert Sharon Lewin of the Peter Doherty Institute for Infection and Immunity in Melbourne, Australia.
Pembrolizumab works by reactivating worn-out immune cells that express a bunch of proteins on their surface, including one marker called PD1. Past research from Lewin and colleagues has shown HIV co-opts these same 'exhaustion' markers to sneak into hibernation and lie undetected.
Blocking PD1 with pembrolizumab reawakens tired T cells whose job is to seek and destroy cancer cells. Researchers had wondered if the drug might also unlock reservoirs of HIV lying dormant in immune cells and bring the virus out of hiding.
Until now, there have only been a handful of case reports showing immunotherapies like pembrolizumab might flush HIV out of immune cells in people with HIV – because although they have an increased risk of developing cancer, people with HIV in need of anti-PD1 treatments for their cancer are very rare.
The drug "did not eradicate HIV in this study" but the result "informs efforts to manipulate T cells to cure HIV," medical oncologist and lead author Thomas Uldrick of the Fred Hutchinson Cancer Research Center said on Twitter.
Bloods were collected from the 32 participants before and after treatment with pembrolizumab, and the samples were analyzed to see how much of the virus's genetic material was detectable in immune cells and blood plasma.
Although most people in the trial still had undetectable levels of HIV in their blood plasma, the researchers did find evidence that a week after the first treatment, a modest but significant level of the virus had been coaxed out of hibernation and started replicating again. Six treatment cycles later, T cells containing HIV that was ready to replicate were also more often detected in some participants.
More research is needed to figure out exactly how anti-PD1 drugs like pembrolizumab modify the immune response and act on HIV-specific T cells. The team is pursuing these questions "in the hope that as well as reversing HIV latency, it will also rev up the immune system to kill the HIV-infected cells in the way it does with cancer," says Lewin.
That remains to be seen, although given how familiar scientists are with pembrolizumab, there is "potential for this and other similar treatments to develop a pathway towards a pragmatic HIV cure," Kirby Institute virologist Stuart Turville told Melissa Davey at The Guardian. He was not involved in the study.
Lewin added, however, that immunotherapies could form part of a multi-pronged treatment approach that she hopes could help the nearly 2 million people diagnosed with HIV every year. "I think it's very unlikely a single drug or intervention is going to cure HIV," she told Davey.
Researchers will also need to further investigate and weigh up the drug's known side effects, which may be tolerable for people with a life-threatening illness such as cancer, but have thus far been a barrier to testing immunotherapies in otherwise healthy people living with HIV.
"In HIV, the situation is very different," says Lewin. "People can now live normal and healthy lives with HIV, so any intervention for a cure must have very low toxicity."
To understand more, the researchers are about to embark on another trial looking at the effects of anti-PD1 therapy on blood cells and lymph nodes to try and find the lowest, safest dose for people living with HIV who don't have cancer, Lewin says.
The current study was published in Science Translational Medicine.