A loss of controlled inhibition of overly excited brain cells might explain how a common knock-out anesthesia drug works.
A new animal study led by researchers from the Massachusetts Institute of Technology (MIT) has found that propofol, a sedative used to safely lull people into unconsciousness for medical procedures, disrupts the brain's normal ability to regain control of highly excitable neurons.
"The brain has to operate on this knife's edge between excitability and chaos," explains MIT neuroscientist and senior study author Earl Miller.
"It's got to be excitable enough for its neurons to influence one another, but if it gets too excitable, it spins off into chaos. Propofol seems to disrupt the mechanisms that keep the brain in that narrow operating range."
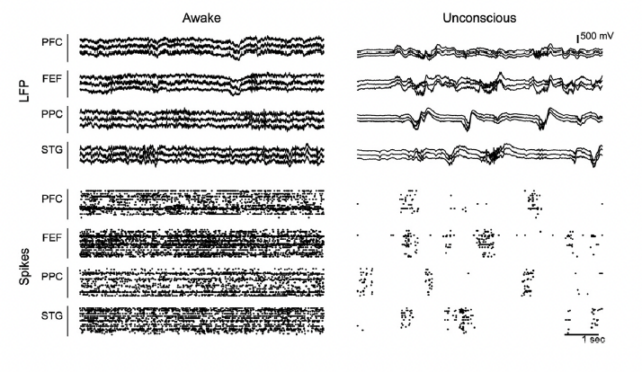
The team measured the brain activity of a pair of rhesus macaque monkeys (Macaca mulatta) for one hour as they lost and regained consciousness after being dosed with propofol .
Hundreds of electrodes placed on the animals' scalps recorded electrical activity in four brain regions while the macaques were 'asleep' and awake. The researchers then analyzed the data with a new technique they developed for quantifying the stability, or robustness, of brain activity.
Normally, brain activity spikes when inputs are received, and then levels out. But once propofol dosing began, the animals' brain activity took longer to return to baseline and then became increasingly excitable as anesthesia deepened, until the animals lost consciousness.
The researchers suggest propofol acts on inhibitory neurons that would otherwise dull overzealous brain activity and return the system to stability after disturbances. This loss of inhibition leads to escalating instability and eventually a loss of consciousness – as if the system gets tripped and the brain can no longer process information.
Of course, this is just one new theory. Despite nearly two centuries of use, we have only a fuzzy idea of how anesthetics work.
A landmark discovery in 1994 suggested anesthetics act on proteins involved in cell signaling, rather than the fatty molecules that make up cell membranes. In 2018, Australian neuroscientists also discovered that propofol messes with a key protein that nerve cells use to communicate with each other.
Yet as recently as 2020, researchers were still finding that other commonly used anesthetic drugs meddled with lipid membranes – so it's darn complicated.
Zooming out to look at entire brain networks, scientists have made progress in the past few decades in identifying distinct brain circuits involved in either the loss of consciousness induced by anesthetics, or awakening from it when the drugs wear off.
In a similar vein, the researchers behind this latest study looked at patterns in overall brain activity, extrapolating from the electrode measurements and using a computer model to test their theory.
While their findings suggest propofol inhibits inhibitory neurons, a study of fruit flies published just last month found another anesthesia drug has somewhat of an opposite effect, targeting excitatory neurons but in a different way.
Rather than unleashing excitatory neurons, isoflurane appears to stop excitatory neurons from communicating, 'silencing' them.
These differences might be explained by the fact the studies looked at different anesthetic drugs: isoflurane, which is inhaled, and propofol, which is injected intravenously – and are known to have differing effects on neurons and cell receptors.
Even so, the team thinks there might still be some commonalities between anesthetic drugs and their effects on the stability of brain-wide dynamics.
"If you find common mechanisms at work across different anesthetics, you can make them all safer by tweaking a few knobs, instead of having to develop safety protocols for all the different anesthetics one at a time," says Miller.
"You don't want a different system for every anesthetic they're going to use in the operating room. You want one that'll do it all."
The study has been published in Neuron.