A common blood condition associated with an increased risk of several diseases unexpectedly appears to lower the risk of Alzheimer's disease.
People with clonal hematopoiesis of indeterminate potential (CHIP) are 10 times more likely to develop blood cancers and twice as likely to end up with heart and liver conditions. So when Stanford University cell biologist Hind Bouzid and colleagues set out to see how this condition messed with Alzheimer's, this was not the outcome they were expecting.
"We were surprised to find that CHIP was actually associated with a substantially lower risk of Alzheimer's disease," says Stanford pathologist Siddhartha Jaiswal.
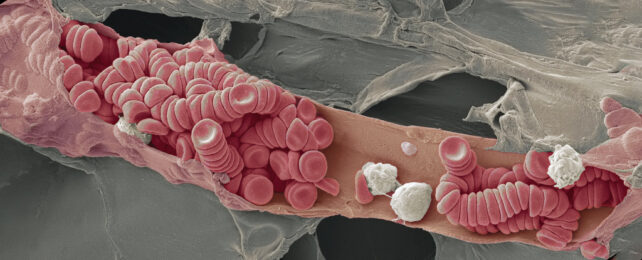
CHIP is often an age-related process. It arises when a blood cell parent (a stem cell) that lives in our bone marrow ends up with a mutation allowing it to create mutant blood cells stronger than their peers. CHIP can form in otherwise healthy people and doesn't have noticeable symptoms but exacerbates other conditions.
As these blood cells can outcompete others, this genetically unique clone strain can replace nearly 100 percent of a person's blood over time.
Analyzing the DNA of blood cells from 1,362 people with Alzheimer's and 4,368 individuals without, Bouzid and the team found a 30–50 percent lower risk of Alzheimer's in people with the blood mutation. This is a similar degree of protection as a genetic variant known to reduce Alzheimer's, Jaiswal explains.
It also suggests the mutation impacts tissues other than red blood cells. The researchers took a closer look guided by past research that previously found a link with other cells derived from bone marrow (collectively known as myeloid tissue).
Thanks to 12 donors, eight who had lived with CHIP and four without, the team identified such CHIP-carrying myeloid cells in brain tissue. Seven of eight CHIP carriers had an increase in immune cells.
Usually, the white blood cells that engulf foreign invaders in the brain are microglia, which are produced within the brain's connective tissue. But these cells that originated from bone marrow had somehow snuck into the brain and taken on the immune system role of microglia.
"This suggests that cells are migrating from the blood into the brain," says Jaiswal. "It's a remarkable finding."
"One hypothesis is that the mutations that promote a growth advantage in blood stem cells also promote microglial expansion and activity, boosting microglia's ability to fight the conditions that lead to brain disease," Jaiswal continues.
Dysfunction of the brain's immune system plays a likely role in Alzheimer's. So if bone marrow-derived imposters are indeed entering the brain in CHIP carriers, they could be outcompeting the faulty brain-derived microglia in Alzheimer's patients and taking on the roles the microglia are now neglecting.
Strangely, the team didn't find consistent epigenetic changes that would explain these effects when they attempted to look. This could be due to the small sample size or that it takes some other factor to trigger them, which has been seen in other disease states, they explain.
So they can't yet directly pin the protection to the imposter microglia.
While there's still a lot to sort out, the multiple lines of evidence Bouzid and colleagues have provided suggest that marrow-derived cells with the CHIP mutations grant some protection from Alzheimer's disease.
This research was published in Nature Medicine.