A case study of a US man who lost vision in his right eye for two days could provide further insight into how SARS-CoV-2 messes with our immune system in ways that cause the body to attack itself.
Like tens of thousands of people in the US each day, an unnamed patient aged in his 70s experiencing a runny nose was given a diagnosis of COVID-19. Three weeks later he presented himself to hospital with a whole other batch of symptoms.
In a report detailed by a team of doctors from the Columbia University Vagelos College of Physicians and Surgeons in New York, the man had recovered from the worst of his bout of COVID-19, only to come down with a headache a week later.
This was soon followed by fading vision in his right eye, to the point he could only make out broad motions. Any movement made with that eye also induced severe pain.
Cases of impeded vision following a SARS-CoV-2 infection aren't common, but aren't unheard of either, with a number of case reports hinting at potential links. Where this case stands out is in the combination of symptoms, including those intense headaches and discomfort in the eye itself.
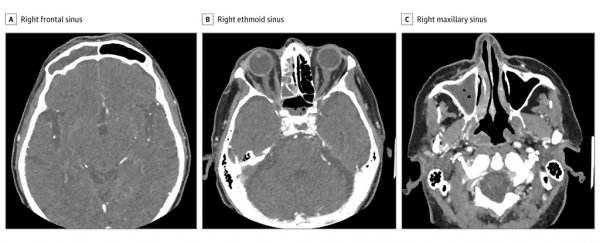
A CT scan quickly revealed the source of the patient's agony were seriously inflamed sinuses extending down the right side of his face. The case was so serious, it was causing the bone itself to erode, necessitating an emergency procedure to remove as much of the inflamed material as possible from each of the cavities.
The surgery seemed to be a winning strategy, at first. But soon the pain returned and his vision once again worsened.
Tissue cultures showed the presence of a bacterium called Streptococcus constellatus. Typically at home in the intestines and oral cavity, this happy human bug can turn particularly nasty when relocated to other areas of the body.
Still, the antibiotics should have been putting a lid on this particular microbe's appetite for destruction.
Further investigation revealed a prevalence of an active type of white blood cell on the prowl, one that typically churns out a strange little antibody called IgG4. Far from your typical antibody, it's capable of reassembling itself in clever ways that turn them into asymmetrical patchworks.
It's also got a reputation for causing its own litany of problems through IgG4-related disease (RD) – an autoimmune condition that can strike just about any part of the body, whipping up inflammation and causing all manner of pain and misery in the form of highly fibrotic lesions.
With a diagnosis of IgG4-related rhinosinusitis, the patient was given a course of steroids and was soon back on the path to good health and clear vision. Three weeks later he was completely recovered.
While it might make for a half-decent episode of House, the discovery also leaves us with an interesting question. Could the patient's infection with SARS-CoV-2 have played a role? Or was it just a series of unrelated, if unfortunate events?
There is a possible link. While the cause of IgG4-RD isn't known, there are often suspiciously large numbers of another kind of white cell hanging about IgG4-RD lesions, called cytotoxic CD4-positive T-cell.
If this were a crime show, there'd be a scene now where a SARS-CoV-2-sensitive CD4+ T-cell was dragged into the interrogation room and badgered over why it was also found hanging around inside patients hospitalized with COVID-19.
We know SARS-CoV-2 is a mastermind when it comes to messing with our immune response. It's no great leap to add one more crime against immunity to its rap sheet.
Yet even taking into account an earlier medical case study hinting at the same potential link between IgG4-RD and COVID-19, it's just too soon to draw any solid conclusions between the two diseases.
So far into this global pandemic, with so many cases at hand, it can be hard to tell rare coincidences apart from meaningful connections.
This research was published in JAMA Otolaryngology-Head & Neck Surgery.