A new study on mice suggests that some antipsychotic drugs could also help us tackle the most common form of meningitis.
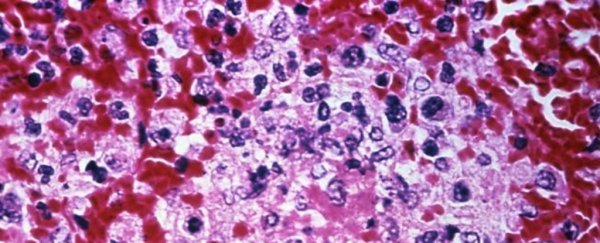
Bacterial meningitis (Neisseria meningitidis) is a serious infection that causes dangerous swelling in the tissue around the brain and spinal cord.
Each year, over 30,000 cases are reported. While most patients recover with antibiotics, if the disease is left untreated, it can cause severe brain damage and even death, sometimes within just a few hours.
Now, a team of scientists from the Institut Cochin in Paris think they've found a better way to treat this disease. Using mouse models, their research shows that a class of antipsychotics, called phenothiazines can stop meningitis from sticking - quite literally.
The drugs are said to work within minutes, disabling the bacterium's long, sticky arms, called Type IV pili. Without these crucial appendages, the bacterium can no longer move, clump together, or cling to blood vessels as easily.
"These compounds exert a strong protective effect," the authors write.
"They reduce meningococcal colonisation of the human vessels and prevent subsequent vascular dysfunctions, intravascular coagulation and overwhelming inflammation, the hallmarks of invasive meningococcal infections. Finally, they reduce lethality."
The medicine works by disarming but not exactly killing the infection; that's where antibiotics can still play a role. When standard antibiotics are used in conjunction with these antipsychotics, the authors say that their efficiency only grows stronger.
As such, it's hoped that together, the two treatments could disrupt existing clumps of the bacterium in humans (which antibiotics cannot currently do) and let the antibiotics kill the infection at play.
Obviously, human clinical trials will be needed before we know if this is an effective treatment for meningitis, but the authors are hopeful given that the drug can already be used on humans.
"It is therapeutically safe with few side effects when used in moderation, as proven by the 60 plus years it has been in use," they write.
"We showed that it reduced vascular lesions and improved mouse survival in the absence of antibiotic treatment when administered early during the infection."
This study has been published in Nature Microbiology.