A drug developed for type 2 diabetes has "significantly reversed memory loss" in mice with Alzheimer's disease, and researchers now want to test it on humans.
The treatment is exciting for scientists because it works by protecting the brain cells attacked by Alzheimer's disease in three separate ways, rather than relying on a single approach.
And seeing as the drug has already been tested and approved for use in humans, it's something that could hit the market a lot faster than other experimental treatment options.
The results have only been seen in mice so far, but the drug "holds clear promise of being developed into a new treatment for chronic neurodegenerative disorders such as Alzheimer's disease," said senior author Christian Hölscher of Lancaster University in the UK.
"With no new treatments in nearly 15 years, we need to find new ways of tackling Alzheimer's," said Doug Brown from UK organisation, Alzheimer's Society.
"It's imperative that we explore whether drugs developed to treat other conditions can benefit people with Alzheimer's and other forms of dementia. This approach to research could make it much quicker to get promising new drugs to the people who need them."
Previous research had already established a link between type 2 diabetes and Alzheimer's - type 2 diabetes is a risk factor for Alzheimer's, and it also appears to make the disease progress more rapidly.
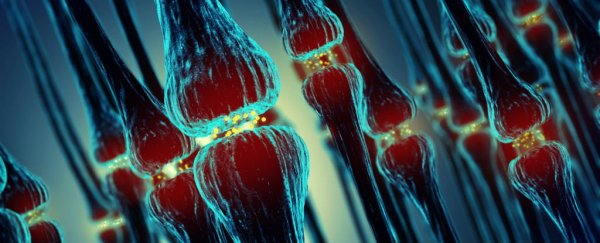
This could be a result of insulin not getting to the cells properly - insulin is a growth factor which is known to protect brain cells, and insulin resistance has been observed in Alzheimer's disease brains, as well as being the biological mechanism behind type 2 diabetes.
So researchers have been investigating whether drugs that treat type 2 diabetes might also benefit Alzheimer's symptoms for a while now.
They've seen previous success in humans with an older diabetes drug known as liraglutide. But this is the first 'triple agonist' drug that's been tested.
The drug, which is referred to only as 'triple receptor agonist', or TA, in the paper, acts in multiple ways to protect the brain from degeneration, by activating GIP-1, GIP, and glucagon receptors at the same time.
Seeing as growth factor signalling has been shown to be impaired in the brains of Alzheimer's patients, the idea was that the drug might help re-stimulate damaged brain cells and protect against further damage.
The researchers tested the drug in mice that had been genetically engineered to have Alzheimer's disease.
They used a maze to measure the animal's learning and memory formation, and found that the drug "significantly reversed the memory deficit," the researchers write.
The drug also:
- enhanced levels of a brain growth factor which protects nerve cell functioning
- reduced the amount of toxic amyloid plaques in the brain
- reduced both chronic inflammation and oxidative stress
- slowed down the rate of nerve cell loss
"These very promising outcomes demonstrate the efficacy of these novel multiple receptor drugs that originally were developed to treat type 2 diabetes but have shown consistent neuro- protective effects in several studies," said Hölscher.
There's still a long way to go before it's clear whether or not this drug will have the same effect in humans, and whether it's the best option to move forward with.
"Further dose-response tests and direct comparisons with other drugs have to be conducted in order to evaluate if this new [drug] is superior to previous ones," Hölscher added.
But the fact that this multi-approach drug has shown such promising results so far is incredibly exciting, and is a great way to start 2018.
After all, more than 5 million Americans are already living with Alzheimer's, and by 2050 that number could be as high as 16 million. So we definitely need new treatment options.
The research has been published in Brain Research.