Vaccines ensure bouts of COVID are far less deadly than they were at the pandemic's start, yet multiple studies now suggest even seemingly mild cases of the coronavirus have a cost. With every single infection, our risk of long COVID increases.
While this risk starts (relatively) low for most of us, particularly those vaccinated and in younger people or children, there are concerning signs it may not stay low. If each new invasion of our bodies allows this insidious virus a greater chance to cause damage, such small risks will eventually add up to a big one.
Even if you only experience the symptom of the initial infection mildly.
"Each subsequent COVID infection will increase your risk of developing chronic health issues like diabetes, kidney disease, organ failure and even mental health problems," physician Rambod Rouhbakhsh warned journalist Sara Berg in an American Medical Association podcast earlier this year.
"This dispels the myth that repeated brushes with the virus are mild and you don't have to worry about it. It is akin to playing Russian roulette."
Long COVID is defined as a multisystem disease that have a devastating effect on any organ system, with potentially lifelong consequences. Rates of long COVID among people who have contracted SARS-CoV-2 vary controversially between studies and regions, from about 10 percent to a staggering 50 percent of people who've had the virus reported as having long term symptoms.
Global estimates suggest 65 million people now suffer from long COVID. Luckily, children currently appear to be impacted at much lower rates, but they're not entirely spared either.
So epidemiologist Benjamin Bowe and colleagues followed 138,818 US veterans with SAR-CoV-2 infections across 2 years, to learn more. Their data demonstrates that on reinfection patients had increased risk of long COVID in multiple organ systems.
The adverse health effects from two infections are worse than one, and three infections worse than two, the researchers explain. This means long COVID is cumulative, at least within this group of people and with this number of re-infections.
As their research is only based on US veterans affairs patients, it may not translate to everyone, but this is not the only study to find this concerning trend.
A study with much broader sampling involving people aged 18 and over across 10 Canadian provinces points to the same conclusion:
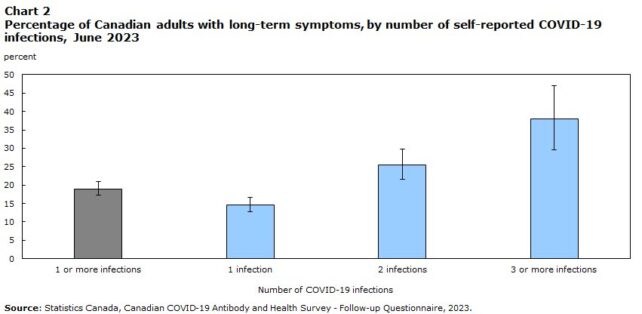
"The study adds to a growing body of evidence around the association between COVID-19 reinfection and the reporting of long-term symptoms," McGill University statistician Sianne Kuang and team write.
Another study, which has yet to be peer reviewed, used data recorded from 1.5 million people in the US to compare severities of initial and subsequent infections. They also note an increase in long COVID after reinfections in the variants following Delta and Omicron.
Whether this is down to reinfection in general or due to changes in newer SARS-Cov-2 strains is still unclear. What's more, Kuang and team caution the studies demonstrating this increase in risk are still "limited in number and generalizability."
However we also know the virus changes our immune systems. It preys on our memory T cells which are critical in forming long term immunity. SARS-Cov-2 forces its way into these cells and causes them to activate the cell's self-destruction programming and essentially implode.
Whether we experience a mild or severe COVID infection, COVID depletes our T cells. This is only one of the long term consequences of COVID, and may contribute to more severe and frequent outbreaks of other diseases like pneumonia and RSV.
Now, approaching the holiday season, wastewater testing indicates many countries, including in the US, are experiencing large new surges of COVID infections. Higher than ever in some places like Germany.
It seems allowing this rapidly mutating pathogen to run rampant has provided it with the perfect laboratory to keep testing out random gene mutations until SARS-CoV-2 stumbles on one that can get past our next line of defenses and out-competes the other strains.
The new JN.1 strain, also called Pirola, has managed just that. A single mutation appears to have made it harder for our immune systems to capture and thwart, meaning past vaccines and infections are no longer as protective.
Early signs indicate the most updated XBB.1.5 vaccines may have better luck against Pirola.
In light of long COVID possibly being cumulative, many of those involved with the disease, from clinicians and scientists to disability advocates and journalists, are so concerned they've signed an open letter to US President Biden urging for more support for the people facing this condition.
