The vagina is an internal organ with a complex ecosystem, influenced by circulating hormone levels which change during the menstrual cycle, pregnancy, breastfeeding and menopause.
Around and after menopause, there are normal changes in the growth and function of vaginal cells, as well as the vagina's microbiome (groups of bacteria living in the vagina).
Many women won't notice these changes. They don't usually cause symptoms or concern, but if they do, symptoms can usually be managed.
Here's what happens to your vagina as you age, whether you notice or not.
Let's clear up the terminology
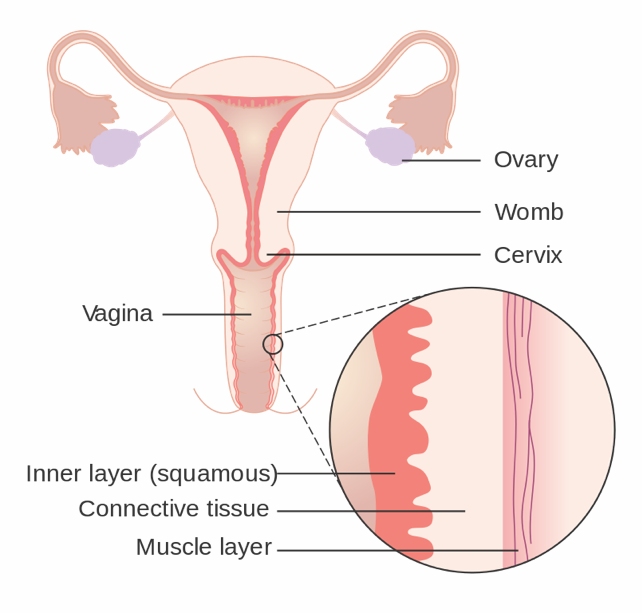
We're focusing on the vagina, the muscular tube that goes from the external genitalia (the vulva), past the cervix, to the womb (uterus). Sometimes the word "vagina" is used to include the external genitalia. However, these are different organs and play different roles in women's health.
What happens to the vagina as you age?
Like many other organs in the body, the vagina is sensitive to female sex steroid hormones (hormones) that change around puberty, pregnancy and menopause.
Menopause is associated with a drop in circulating oestrogen concentrations and the hormone progesterone is no longer produced. The changes in hormones affect the vagina and its ecosystem. Effects may include:
- less vaginal secretions, potentially leading to dryness
- less growth of vagina surface cells resulting in a thinned lining
- alteration to the support structure (connective tissue) around the vagina leading to less elasticity and more narrowing
- fewer blood vessels around the vagina, which may explain less blood flow after menopause
- a shift in the type and balance of bacteria, which can change vaginal acidity, from more acidic to more alkaline.
What symptoms can I expect?
Many women do not notice any bothersome vaginal changes as they age. There's also little evidence many of these changes cause vaginal symptoms. For example, there is no direct evidence these changes cause vaginal infection or bleeding in menopausal women.
Some women notice vaginal dryness after menopause, which may be linked to less vaginal secretions. This may lead to pain and discomfort during sex.
But it's not clear how much of this dryness is due to menopause, as younger women also commonly report it. In one study, 47% of sexually active postmenopausal women reported vaginal dryness, as did around 20% of premenopausal women.
Other organs close to the vagina, such as the bladder and urethra, are also affected by the change in hormone levels after menopause. Some women experience recurrent urinary tract infections, which may cause pain (including pain to the side of the body) and irritation. So their symptoms are in fact not coming from the vagina itself but relate to changes in the urinary tract.
Not everyone has the same experience
Women vary in whether they notice vaginal changes and whether they are bothered by these to the same extent. For example, women with vaginal dryness who are not sexually active may not notice the change in vaginal secretions after menopause. However, some women notice severe dryness that affects their daily function and activities.
In fact, researchers globally are taking more notice of women's experiences of menopause to inform future research. This includes prioritising symptoms that matter to women the most, such as vaginal dryness, discomfort, irritation and pain during sex.
If symptoms bother you
Symptoms such as dryness, irritation, or pain during sex can usually be effectively managed. Lubricants may reduce pain during sex. Vaginal moisturisers may reduce dryness. Both are available over-the-counter at your local pharmacy.
While there are many small clinical trials of individual products, these studies lack the power to demonstrate if they are really effective in improving vaginal symptoms.
In contrast, there is robust evidence that vaginal oestrogen is effective in treating vaginal dryness and reducing pain during sex. It also reduces your chance of recurrent urinary tract infections. You can talk to your doctor about a prescription.
Vaginal oestrogen is usually inserted using an applicator, two to three times a week. Very little is absorbed into the blood stream, it is generally safe but longer-term trials are required to confirm safety in long-term use beyond a year.
Women with a history of breast cancer should see their oncologist to discuss using oestrogen as it may not be suitable for them.
Are there other treatments?
New treatments for vaginal dryness are under investigation. One avenue relates to our growing understanding of how the vaginal microbiome adapts and modifies around changes in circulating and local concentrations of hormones.
For example, a small number of reports show that combining vaginal probiotics with low-dose vaginal oestrogen can improve vaginal symptoms. But more evidence is needed before this is recommended.
Where to from here?
The normal ageing process, as well as menopause, both affect the vagina as we age.
Most women do not have troublesome vaginal symptoms during and after menopause, but for some, these may cause discomfort or distress.
While hormonal treatments such as vaginal oestrogen are available, there is a pressing need for more non-hormonal treatments.
Dr Sianan Healy, from Women's Health Victoria, contributed to this article.![]()
Louie Ye, Clinical Fellow, Department of Obstetrics and Gynecology, The University of Melbourne and Martha Hickey, Professor of Obstetrics and Gynaecology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
