When dealing with cancer, finding the most effective treatments as early on as possible can be vital. A new blood test could help doctors determine just that.
Scientists have come up with a way of analyzing blood that tells them within 24 hours whether or not targeted cancer therapy (aimed directly at specific molecules) is having an effect on tumor growth. Such a quick turnaround means that the treatment can be quickly adapted or rethought.
It's called extracellular vesicle monitoring of small-molecule chemical occupancy and protein expression (ExoSCOPE), and it works by looking for extracellular vesicles (EVs) in the blood – tiny particles released by cells. In this case, cancer cells that have been hit by a drug will secrete EVs with traces of that drug in them.
"Conventional procedures such as tumor imaging are not only expensive but also delayed," says biophysicist Shao Huilin, from the National University of Singapore (NUS). "For these methods, treatment effectiveness can only be determined after weeks.
"Using the ExoSCOPE, we can directly measure the outcomes of drug effectiveness within 24 hours of treatment initiation. This will significantly reduce the time and cost for cancer treatment monitoring."
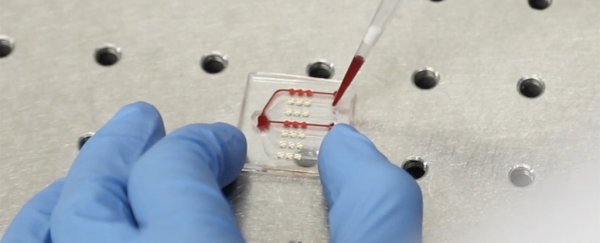
EVs are at least a hundred times smaller than the diameter of human hairs. They can't be seen by standard microscopes, but using a special sensor setup involving millions of gold nanorings, the scientists were able to amplify the drug signals the EVs were giving off.
Through a sophisticated analysis of the light signals given off by the collected blood sample, the ExoSCOPE system can indicate if the drugs have reached their target in the body.
Even better, the new setup is able to monitor drug dynamics over time, checking up on how treatments are either working or being met with resistance. It gives medical professionals a comprehensive picture in a very short period of time.
"This method requires only a tiny amount of blood sample for the analysis and each test takes less than one hour to complete," says Huilin. "So, it is less invasive and yet more informative."
"In this way, doctors could monitor a patient's response to treatment more regularly during the course of the treatment, and make timely adjustments to customize the treatment for better outcomes."
In a clinical trial involving 106 patients with lung cancer, the ExoSCOPE scored a 95 percent accuracy rate when determining drug effectiveness, compared with the current gold standard of tumor measurement – but it did so in a much shorter time.
The study shows the many different ways scientists are making progress when it comes to tackling cancer, not only in developing treatments but in making sure those treatments work, in reducing remission risk, and in spotting cancers earlier to begin with.
Having worked on developing the ExoSCOPE for the past two years, now the team wants to expand its reach to cover more types of diseases and to take in more types of treatment. The technology could be in use in around three years.
"Current technologies to measure drug-target interactions require complex processing and invasive tissue biopsies, limiting their clinical utility for cancer treatment monitoring," says chemical biologist Sijun Pan, from NUS.
"By using specially designed chemical probes, our platform is highly sensitive in capturing and labeling EVs in a small blood sample in order to assess drug-target interactions."
The research has been published in Nature Nanotechnology.