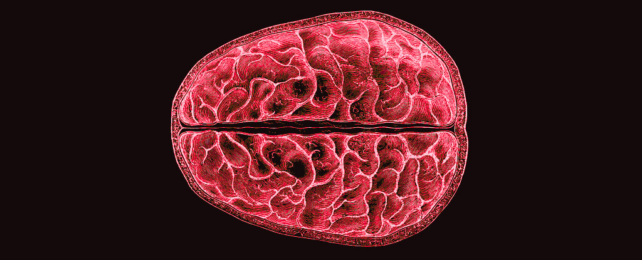
The constant ebb and flow of hormones that guide the menstrual cycle don't just affect reproductive anatomy. They also reshape the brain, and a new study has given us insight into how this happens.
Led by neuroscientists Elizabeth Rizor and Viktoriya Babenko of the University of California Santa Barbara, a team of researchers tracked 30 women who menstruate over their cycles, documenting in detail the structural changes that take place in the brain as hormonal profiles fluctuate.
The results, which are yet to be peer-reviewed but can be found on preprint server bioRxiv, suggest that structural changes in the brain during menstruation may not be limited to those regions associated with the menstrual cycle.
"These results are the first to report simultaneous brain-wide changes in human white matter microstructure and cortical thickness coinciding with menstrual cycle-driven hormone rhythms," the researchers write.
"Strong brain-hormone interaction effects may not be limited to classically known hypothalamic-pituitary-gonadal-axis (HPG-axis) receptor-dense regions."
People who menstruate will experience some 450 or so periods during the course of their lifetimes, so it would be nice to know the different effects they can have on the body, really.
However, although it is something that happens to half the world's population for half their lives, research has been somewhat lacking. Who knows why. Total mystery. Seriously.
Most of the research on the hormonal effect on the brain has been focused on brain communication during cognitive tasks, not the actual structures themselves.
"Cyclic fluctuations in HPG-axis hormones exert powerful behavioral, structural, and functional effects through actions on the mammalian central nervous system," Rizor, Babenko, and their team note. "Yet, very little is known about how these fluctuations alter the structural nodes and information highways of the human brain."
The microstructure of white matter – the fatty network of neuronal fibers that transfer information between regions of gray matter – has been found to change with hormonal shifts, including puberty, oral contraception use, gender-affirming hormone therapy, and post-menopausal estrogen therapy.
To address the menstruation gap in our understanding, the team took MRI scans of their subjects during three menstrual phases: menses, ovulation, and mid-luteal. At the time of each of these scans, the researchers also measured the participants' hormone levels.
The results showed that, as hormones fluctuate, gray and white matter volumes change too, as does the volume of cerebrospinal fluid.
In particular, just before ovulation, when the hormones 17β-estradiol and luteinizing hormone rise, the brains of the participants showed white matter changes suggesting faster information transfer.
Follicle-stimulating hormone, which rises before ovulation, and helps stimulate the ovary follicles, was associated with thicker gray matter.
Progesterone, which rises after ovulation, was associated with increased tissue and decreased cerebrospinal fluid volume.
What this means for the person driving the brain is unknown, but the research lays the groundwork for future studies, and perhaps understanding the causes of unusual but severe period-related mental health problems.
"Although we do not currently report functional consequences or correlates of structural brain changes, our findings may have implications for hormone-driven alterations in behavior and cognition," the researchers write.
"Investigation of brain-hormone relationships across networks is necessary to understand human nervous system functioning on a daily basis, during hormone transition periods, and across the human lifespan."
The team's paper is available on bioRxiv.