Like a nightmarish, post-apocalyptic plot, rising temperatures are causing fungi to mutate in ways that not only make them hyper-infectious but drug-resistant, too.
This is deeply concerning as our world warms, Nanjing Medical University researcher Jingjing Huang and colleagues warn.
"The danger and importance of new fungal pathogens is believed to be seriously underestimated," they write in their new paper.
"Temperature-dependent mutagenesis can enable the development of pan-drug resistance and hypervirulence in fungi, and support the idea that global warming can promote the evolution of new fungal pathogens."
Fungal infections already cause around 3.75 million deaths annually, despite most species preferring much lower temperatures than those found within our bodies.
But previous research suggests that forcing fungi to adapt to warmer environments can completely alter their physiology.
Scientists recently identified the first known fungi likely to have emerged as a pathogen due to climate change: Candida auris. As other fungi become more heat tolerant like C. auris is thought to have, more species will find mammalian bodies a temptingly protective shelter within which they can flourish.
So scouring records of fungal infections from 96 hospitals in China between 2009 and 2019 Huang and team identified a group of fungi that had never been known in humans before. Rhodosporidiobolus appeared independently in two unrelated cases.
Strain NJ103 was isolated from a 61-year-old immunosuppressed man, who died of multiple organ failure despite fluconazole and caspofungin antifungal treatments. Strain TZ579 was isolated from an 85-year-old man who died of respiratory failure after treatment with fluconazole.
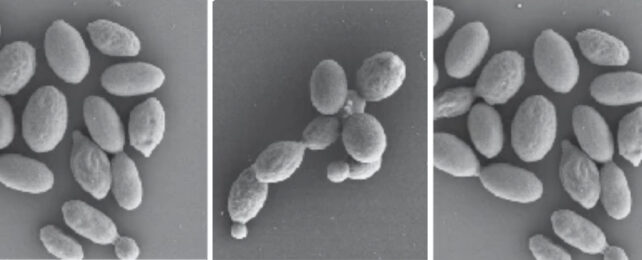
Including those two strains and others from environmental sources the researchers isolated eight different Rhodosporidiobolus species and exposed them to the average human body temperature of 37 °C (98.6 °F) in the laboratory. The species R. fluvialis and R. nylandii both tolerated the heat well – in R. fluvialis, the hot environment even triggered a switch from a single cell yeast form to a more aggressive colonial pseudohyphal phase.
Both species thrived similarly when they were injected into mice.
In its pseudohyphal form, R. fluvialis not only thrived in warmer conditions but were more resistant to immune macrophage cells, killing more of them rather than being killed by them. Both R. fluvialis and R. nylandii are also resistant to three of the most commonly used antifungal medications – fluconazole, caspofungin and amphotericin B.
"R. fluvialis is sensitive to 5-fluorocytosine; however we found that R. fluvialis was able to rapidly generate 5-fluorocytosine-resistant mutants," explain the researchers. "The speed of complete resistance in R. fluvialis was remarkable."
Huang and colleagues did find one substance that Rhodosporidiobolus didn't seem to adapt to as easily: polymyxin B – an FDA-approved bactericide. Unfortunately, this drug is toxic to neurons and kidney cells.
As global temperatures warm, these morphological changes could increase our risk of encountering dangerous fungi in the future. More fungicide options are urgently needed.
This research was published in Nature Microbiology.