Tensions between the brain, the gut, and the makeup of its microbial inhabitants appear to play a critical role in the development of neurodegenerative conditions.
While evidence favoring a link between the microbiota-gut-brain axis (MGBA) and Alzheimer's disease continues to grow, the exact mechanism behind the relationship is still poorly understood.
The puzzle pieces have so far been frustratingly incoherent, involving seemingly unrelated factors as tangled proteins inside nervous tissue to suspect gut microbes to subtle differences in fat-transporting molecules.
Using the largest ever genome-wide association study of human gut microflora, a team of researchers from the US sought out a more explicit relationship between Alzheimer's disease and the mix of organisms living inside the digestive system.
Their analysis uncovered not only a genetic connection between different genera of gut bacteria and a diagnosis of Alzheimer's but also a link between the microbes and a genetic risk factor for the neurodegenerative disorder.
The study further emphasizes the interplay of genetic factors and inflammatory gut microflora in healthy brain function.
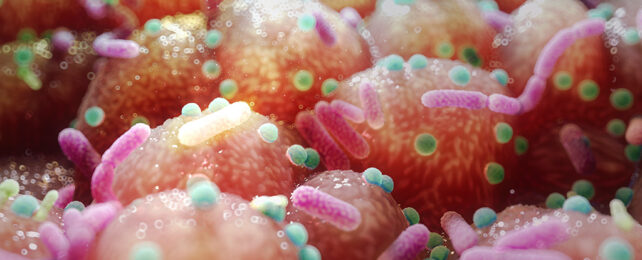
Early in our development, our bodies are colonized by an assortment of bacteria, fungi, and viruses that strike a tentative truce with the immune system. For the most part, this arrangement is mutually beneficial. The microbes get a place to live, and we get a front-line defense of tiny occupants willing to protect their home.
That's not to say the balance is always a harmonious one. Shifts in our immune system can give some species an advantage over others. Likewise, changes in the makeup of microbes – by way of shifts in our diet, for example – can profoundly affect the body's functioning. For better and worse.
The tug-of-war between our microbial census and general health can ripple throughout the body in less than predictable ways, sowing confusion in how distant tissues identify friend and foe.
In recent years, researchers have focused on this complex diplomacy between gut microflora, the immune system, and neurological functioning in an attempt to understand why areas of the brain degenerate and give rise to the symptoms of memory loss and cognitive decline we recognize as Alzheimer's disease.
Observational studies revealed a reduction in the diversity of gut microbes in individuals diagnosed with the condition, while laboratory analyses showed gut bacteria can release chemicals that could induce damaging inflammatory signals in the brain.
Complicating matters is a gene involved in the movement of fats through the blood known as apolipoprotein E (APOE). Of the three versions found in humans, a variant known as E4 appears to be a genetic risk for Alzheimer's. Why this is the case isn't clear, though there's good reason to suspect that having at least one copy of APOE E4 might hold some sway over the composition of our microbial citizens.
This latest exploration of the connections between microbes, APOE E4, and Alzheimer's provides even more compelling evidence of a mechanism at work in the gut.
The team trawled through detailed records of 119 bacterial genera based on a study involving thousands of participants, known as the MiBioGen Consortium.
An initial search of bacterial genes that could be associated with Alzheimer's revealed 20 genera suspected of playing some kind of role in the disease's development. A second hunt through a more constrained sample produced a slightly more certain 10 genera – six of which were fewer among diagnosed patients, and the remaining four being more common.
Of those 10 bacteria genera, four seemed to have a relationship with an APOE allele that is thought to raise the risk of Alzheimer's disease.
One example genus is the Actinobacterium Collinsella, which isn't only associated with Alzheimer's and the APOE variant but rheumatoid arthritis, atherosclerosis, and Type-2 diabetes as well.
The researchers suspect Collinsella's ability to promote the expression of inflammatory messenger hormones, together with its knack for making the gut more permeable, could play a role in exacerbating – if not triggering – neurological damage.
Elevated cholesterol and low-density lipoprotein (LDL) levels found in healthy adults with high numbers of Collinsella further show some link between microbes, fat metabolism, and neurodegeneration.
This is just one avenue for exploration; the research also uncovered 'protective' bacterial groups that could counter inflammation.
Alzheimer's disease is the most common form of dementia, which is projected to affect 150 million people worldwide by the middle of the century, thanks largely to a substantial global population growing older by the year.
Tracing the origins of the illness and understanding its pathology on a fundamental level is vital if we're to find ways to treat or even prevent its symptoms.
This research was published in Scientific Reports.