Up to one in four patients who are unresponsive after suffering serious brain injuries might actually still be conscious – indicating more patients may be aware of their surroundings than previously realized, new research suggests.
This discovery could potentially make huge differences to how care should be managed for those classified as being in a coma, a vegetative state, or a minimally conscious state. These terms may not tell the full story, according to the international team behind the new study.
This state of 'hidden consciousness' is now officially known as cognitive motor dissociation (CMD), where cognitive (or thinking) abilities aren't connected to motor (or movement) abilities. Researchers have been looking into CMD for several years.
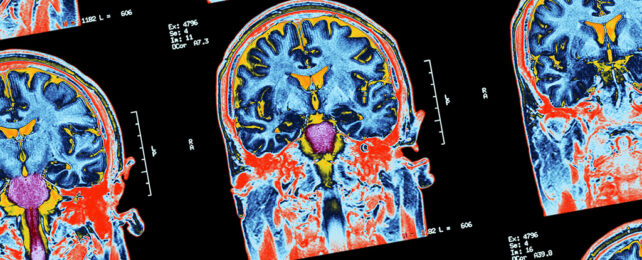
In the new study, signs of consciousness were found through fMRI (functional magnetic resonance imaging) and EEG (electroencephalography) brain scans in 60 out of 241 patients tested, after being given instructions such as "imagine opening and closing your hand".
"Some patients with severe brain injury do not appear to be processing their external world," says neurologist Yelena Bodien from Massachusetts General Hospital.
"However, when they are assessed with advanced techniques such as task-based fMRI and EEG, we can detect brain activity that suggests otherwise.
"These results bring up critical ethical, clinical, and scientific questions – such as how can we harness that unseen cognitive capacity to establish a system of communication and promote further recovery?"
While earlier studies have shown similar results, the new research finds a higher prevalence of CMD, involves the biggest sample yet tested, and is the first to cover multiple locations: Six different sites were included, with data collected across the course of 15 years.
Interestingly, CMD was spotted more often in patients tested with both fMRI and EEG, suggesting a range of tests should be used to look for it.
However, 62 percent of an additional 112 patients who were visibly responding to instructions at the bedside didn't exhibit the expected brain signals showing responsiveness – so the researchers suggest their methods still don't detect everyone with cognitive function.
"To continue our progress in this field, we need to validate our tools and to develop approaches for systematically and pragmatically assessing unresponsive patients so that the testing is more accessible," says Bodien.
Knowing a patient is listening and responding – even if it isn't visible on the surface – can transform the approach of carers and families, when it comes to talking, playing music, and looking for signs of a response.
Previous research suggests that life support systems may be switched off too early in some cases, and we have seen various examples of people waking up from a minimally conscious state long after hope had been lost.
A 2019 study of unresponsive patients found those with CMD have around twice the likelihood of recovering some independent function in the 12 months following acute brain injury.
"We have an obligation to try to reach out to these patients and build communication bridges with them," says neurologist Jan Claassen from the Columbia University Irving Medical Center.
"Having this information gives us the background we need to develop interventions to help them recover."
The research was published in The New England Journal of Medicine.