A major study has investigated how AIDS has evolved since it first infected humans 100 years ago to find that it's becoming weaker and less virulent, and its ability to cause AIDS is slowing down.
Led by a team from the University of Oxford, the research suggests that together with the use of antiretroviral therapies, the rapid evolution of the HIV virus to fight our immune systems has resulted in a less deadly form.
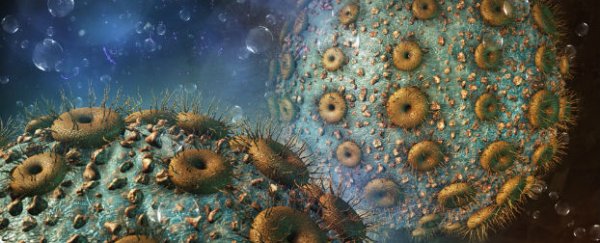
Currently affecting more than 35 million people all around the world, and responsible for the death of 40 million over the past three decades, HIV has been such a devastating virus because of its ability to mutate and disguise itself so fast. It appears to match every move its host's immune system makes, except in a select few patients who are protected by particularly efficient immune systems.
"[Then] the virus is trapped between a rock and hard place, it can get flattened or make a change to survive, and if it has to change, then it will come with a cost," one of the team Philip Goulder told James Gallagher at BBC News.
Gallagher explains that this "cost" affects the virus's capacity to replicate itself, which weakens its ability to cause AIDS in its host, or infect someone else. He reports that some virologists have even suggested that if HIV continues evolving as it has been, eventually it could become "almost harmless" .
The team figured this out by studying HIV in 2,000 women from South Africa and Botswana, in Southern Africa, and comparing the different mutations across the two groups. The rationale was that, as Southern Africa was the epicentre for the virus, the forms affecting people there have had longer to evolve than those in South Africa, where the virus spread at least 10 years later.
According to a press release from the team, certain proteins in our blood called human leukocyte antigens (HLA) were central to their investigation, because they enable the immune system to figure out which proteins are the body's and which belong to the virus. That is, which proteins to attack, and which to leave well alone. "People with a gene for a particular HLA protein called HLA-B*57 are known to benefit from a 'protective effect' to HIV," the team reports. "That is, infected patients with the HLA-B*57 gene tend to progress more slowly than usual to AIDS."
They found that in the Botswana women, the HIV had mutated so much, it had adapted to HLA-B*57, but the cost of all that effort made it less able to replicate. In the South African women, on the other hand, HIV was less able to fight HLA-B*57, but much quicker to replicate, cause AIDS, and infect other people.
"It is quite striking. You can see the ability to replicate is 10 percent lower in Botswana than South Africa and that's quite exciting," Goulder told Gallagher at the BBC. "We are observing evolution happening in front of us and it is surprising how quickly the process is happening. The virus is slowing down in its ability to cause disease and that will help contribute to elimination."
Publishing in the journal Proceedings of the National Academy of Sciences, the team also used a mathematical model to figure out where to go from here, with the help of antiretroviral AIDS therapies. The model showed that the best course of action would be to treat the nastiest forms of the virus in patients with weakened immune systems, and to encourage the evolution of the weaker form.
"This research highlights the fact that HIV adaptation to the most effective immune responses we can make against it comes at a significant cost to its ability to replicate," said Goulder in the press release. "Anything we can do to increase the pressure on HIV in this way may allow scientists to reduce the destructive power of HIV over time."
Sources: BBC News, The University of Cambridge