In the last few years neuroscientists have gotten much better at growing the beginnings of the human brain in the lab. Now, these 'mini-brains' are growing complex enough for us to study neurological disease in its earliest stages.
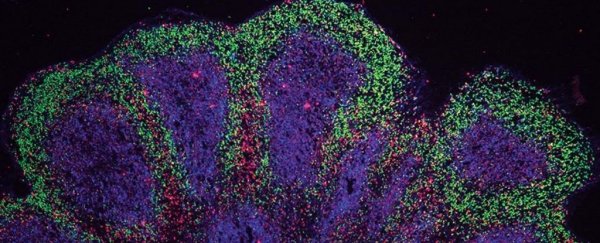
The gray blobs, known as brain organoids, are not capable of consciousness, but they can teach us about the structure, diversity, and interactions of cells in certain parts of the developing brain.
Researchers compare brain organoids to the structure of a fetus' brain after about a dozen weeks of growing. The little blobs can't think, but they can send out tendrils to a muscle and cause contractions. They can't feel, but they can develop rudimentary eye structures.
To get to even that simple level of development takes scientists a lot more time than nature itself. Getting a human's stem cells to proliferate into the millions and grow into something resembling a 'mini-brain' requires bathing it in just the right cocktail of molecules to turn genes on or off at just the right time.
Maintaining them isn't easy, either. Brain organoids derived from the stem cells of those with Parkinson's disease have been grown for about 30 days. For Alzheimer's disease, they've been grown for 84 days.
Researchers at Cambridge have now grown a pea-sized mini-brain to study amyotrophic lateral sclerosis (ALS) for nearly a year, which is a really big step.
ALS, which often overlaps with frontotemporal dementia (ALS/FTD), is a currently untreatable neurodegenerative disease that leads to rapid cognitive decline and paralysis. Because the neurological symptoms don't show up until later in life, scientists know very little about how it starts.
Enter the lab-grown mini-brain, grown using stem cells from patients with ALS/FTD.
One of the big hurdles with growing brain-like clumps in a dish is that as the organoid grows, cells in the middle become deprived of nutrients and stop becoming useful models.
To get around this, some researchers a few years ago started slicing the organoids before bathing them in culture, keeping their models alive for longer periods and for better study.
Researchers at Cambridge did this with their early model of ALS/FTD. In unpublished work, the team claims to have grown their organoids for a total of 340 days.
All that is published so far is 240 days, but within that time, the authors observed changes within two types of brain cells. These changes included cell stress, damage to cell DNA, and changes to how the cell's DNA was ultimately transcribed into proteins.
The destructive changes seemed to impact C9 neurons and another type of neural cells – called astroglia – both of which help manage muscle movement and mental abilities in the real human brain.
"Although these initial disturbances were subtle, we were surprised at just how early changes occurred in our human model of ALS/FTD," says neurologist András Lakatos from the University of Cambridge.
"This and other recent studies suggest that the damage may begin to accrue as soon as we are born. We will need more research to understand if this is in fact the case, or whether this process is brought forward in organoids by the artificial conditions in the dish."
One of the more interesting findings from the ALS/FTD model was that a drug known as GSK2606414f, or GSK for short, could partially suppress some of the neuronal changes that seemed to occur early on in cortex development, including the clumping of toxic proteins, cell stress, and the loss of nerve cells.
Already, the authors say, similar drugs that are better suited to humans are being tested in clinical trials for neurodegenerative diseases. The team hopes their technique of growing organoid models of neurological disease will help identify further potential drug targets in the future.
"We currently have no very effective options for treating ALS/FTD, and while there is much more work to be done following our discovery, it at least offers hope that it may in time be possible to prevent or to slow down the disease process," explains Lakatos.
"It may also be possible in future to be able to take skin cells from a patient, reprogram them to grow their 'mini brain' and test which unique combination of drugs best suits their disease."
We're still a long way from that reality, but looking back, neuroscientists have achieved a lot in just a few short years.
The study was published in Nature Neuroscience.