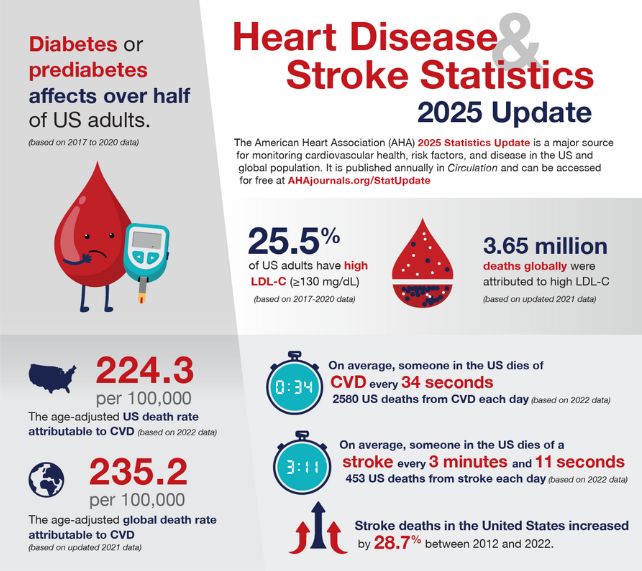
Someone dies of heart disease about every 34 seconds in the US, according to a new report, confirming the often preventable condition as the nation's leading cause of death.
"Those are alarming statistics to me – and they should be alarming for all of us, because it's likely many among those whom we lose will be our friends and loved ones," says physician Keith Churchwell, president of the American Heart Association.
The 2025 Heart Disease and Stroke Statistics Update analyzed the most recent data available, finding a total of 941,652 US deaths in 2022 from cardiovascular disease, which includes all diseases of the circulatory system.
The number of cardiac disease deaths in the 2022 CDC data was followed by the number of deaths from cancer, accidents, and then COVID-19.
"Too many people are dying from heart disease and from stroke which remains the 5th leading cause of death," continues Churchwell. "Together, they kill more people than all cancers and accidental deaths combined."
What's more, known heart disease risk factors, including high blood pressure, diabetes, and obesity continue to rise. If such trends continue hypertension and obesity will impact more than 180 million adults in the US by 2050.
In an accompanying commentary, Harvard University cardiologist Dhruv Kazi notes some of the more recent data, especially for children and adolescents, may be impacted by lifestyle changes imposed by the COVID-19 pandemic.
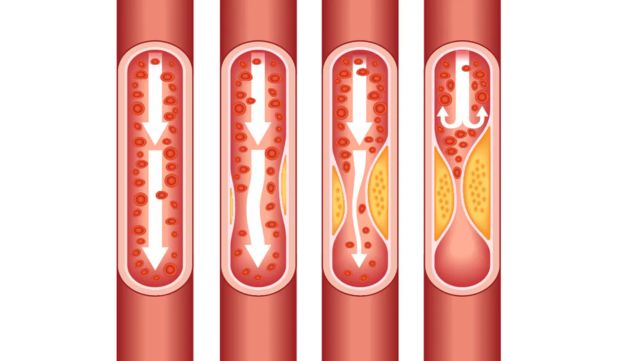
The comprehensive report points out that one of the biggest culprits is poor diet. Most Americans do not eat enough healthy, unprocessed foods. Heavily plant based diets like the Mediterranean or vegetarian diets are recommended for heart health.
Getting enough sleep, exercise, and managing stress and mental health all also contribute.
The report acknowledges that environmental factors, including education, income, and neighborhood availability, greatly impact food and other lifestyle choices. For example, the increasing cost of groceries can dissuade people from making healthy food choices.
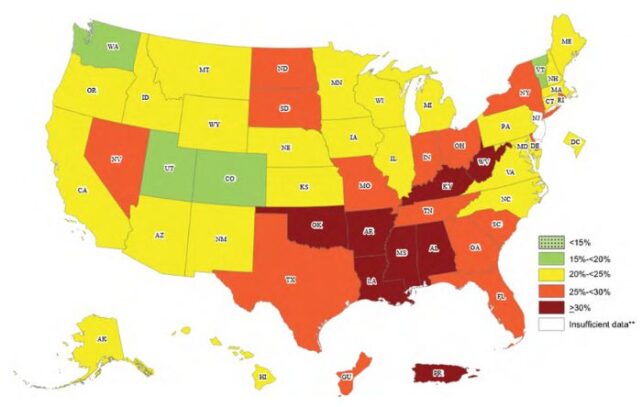
As such, marginalized minority groups continue to face the greatest barriers to healthy heart choices and more heart stressors, as reflected by the heart disease outcomes.
"The age‐adjusted obesity-related cardiovascular mortality was noted to be highest among Black individuals, followed by American Indian individuals or Alaska Native individuals," the report explains.
The good news is that smoking, another major risk factor, has fallen dramatically from 42 percent of the US adult population in the 1960s to 11.5 percent.
"Excess weight now costs us even more lives than smoking – as smoking rates have actually fallen in recent years," says Stanford University cardiologist Latha Palaniappan.
Cholesterol levels have also decreased, suggesting efforts to increase awareness of the risks of high cholesterol are having some effect.
"The disparities in risk and outcomes call for tailored interventions among high-risk populations," urges Kazi. "Simply discovering breakthrough therapies isn't going to be enough – we have to ensure that these therapies are accessible and affordable to people who need them most."
The National Institute for Health recommends getting regular screening tests for heart disease from age 20, especially if you have a family history of heart conditions.
Such screening includes tests for blood pressure, cholesterol, and glucose levels.
"Although we have made a lot of progress against cardiovascular disease in the past few decades, there is a lot more work that remains to be done," says Kazi.
You can read the full report in Circulation.
