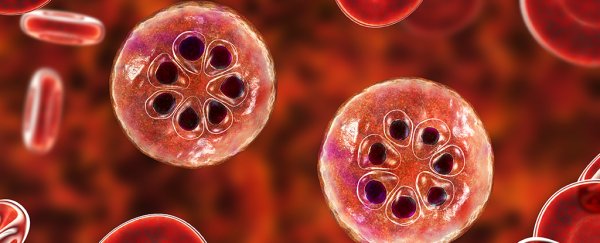
Malaria is an infectious disease caused by species of single-celled parasites invading and destroying red blood cells.
There are four species of Plasmodium protozoan that cause malaria in humans, with two – P. falciparum and P. vivax – responsible for the majority of infections.
Plasmodium parasites reproduce in two ways: asexually inside a host's liver tissue and blood cells; and sexually inside female Anopheles mosquitoes, via specialised Plasmodium sex cells that the insect has consumed with the host's blood.
How do you get malaria?
That means the parasites can only be transmitted through the bite of an infected female Anopheles mosquito, making the insect a vital part of the disease chain. As a result, malaria continues to be endemic in parts of the world where this particular species of mosquito breeds in large numbers, particularly in tropical regions of Africa.
In 2018, nearly 230 million people around the globe suffered from the disease, with just under half a million dying as a result of the infection. More than two-thirds of those were children under the age of five.
An unreferenced claim in a 2002 Nature article suggests as many as half of all people who ever lived might have died as a result of malaria
Though the statistic is surprisingly high, and disputed, malaria's impact on human migration and evolution has most likely been greater than that of any other infectious agent. In fact, the origins of the disease can be traced back to the times of the dinosaurs.
What are the symptoms of malaria?
Roughly one to three weeks after becoming infected, individuals can expect to experience flu-like symptoms that include cycles of sweating and shivering with a fever, headaches, joint pain, and vomiting. In severe cases, skin and eyes can become jaundiced (yellow in appearance) due to impaired liver function.
Taking preventative medicines or having some form of mild immunity can delay symptoms or make them less severe.
If untreated, the disease can give rise to complications including trouble breathing and weakness from anaemia that can put young infants and immunocompromised people at risk of death.
How is malaria treated?
A variety of natural and synthetic drugs have been developed over time to help reduce the chances of malaria parasites establishing an infection. Many medications come with side effects, risk of complications, or increased resistance among species of Plasmodium.
Early diagnosis gives those infected the best chance of recovery, with currently recommended treatments based on the antimalarial compound artemisinin. Combining this medication with other non-artemisinin treatments reduces the risk of resistant strains of Plasmodium evolving.
There has been progress over the years in developing a vaccine to prevent infections. In 2019, a WHO-directed malaria vaccination program in three sub-Saharan African countries distributed one called RTS,S/AS01 (trade name Mosquirix) that targets P. falciparum, the most deadly parasite globally.
By far the most effective means of managing the disease is strict control of its vector, the Anopheles mosquito. Netting, pesticides, and eradication of breeding grounds has helped many communities under threat all but eliminate one of history's oldest diseases.
All Explainer articles are determined by fact checkers to be correct and relevant at the time of publishing. Text and images may be altered, removed, or added to as an editorial decision to keep information current.