The bacteria living inside your mouth could be influencing more than just the health of your gums and teeth. Your brain might also be impacted by these oral colonizers.
In a study of 55 participants with mild cognitive impairment (MCI), those who hosted a relatively high abundance of bacteria from the genus Neisseria in their mouths had better working memory, executive function, and visual attention.
Even among 60 people without cognitive decline, when Neisseria dominated the oral microbiome, working memory scores improved.
The current study, led by researchers at the University of Exeter in the UK, suggests that by promoting certain bacteria in the mouth we could potentially delay cognitive decline. This could be achieved with probiotics or prebiotics that can boost and feed certain microbial communities in the oral cavity within just weeks.
The findings align with other recent studies, which suggest the cause of dementia may be coming from inside the mouth.
In recent years, for instance, poor oral health has emerged as a major risk factor for cognitive decline. Scientists have even found some bacteria linked to gum disease in the brains of those who have died from Alzheimer's.
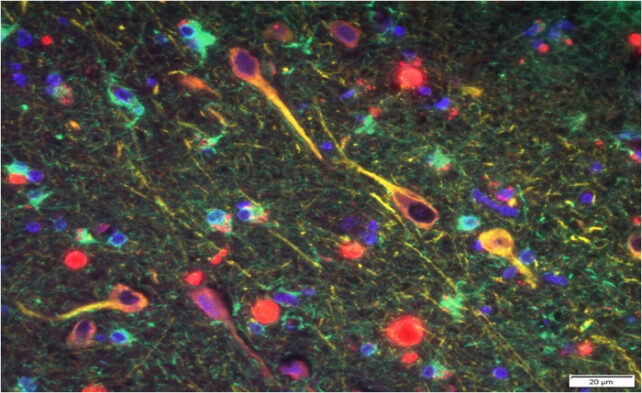
Still, not all microbes in the mouth are necessarily harmful to the brain; some could be protective, too. Similar to bacteria in the gut, a nicely balanced microbiome is key.
The Neisseria genus includes more than 20 species of bacteria, many of which typically live in the nose and mouth quite peacefully and may even confer health benefits.
Recently, studies have found Neisseria bacteria can lower a person's systemic blood pressure by helping to convert nitrate-rich foods (usually vegetables) to nitric oxide.
Nitric oxide is a key signaling molecule in the body, which protects against gum disease and helps control and regulate blood pressure, as well as our cardiovascular response to exercise. It could also help keep the brain healthy.
Based on recent evidence, some neuroscientists suspect nitric oxide may protect the central nervous system by boosting neural plasticity and improving the efficiency and power of neural messages. The signaling molecule may even reduce neural inflammation – a central mechanism of Alzheimer's.
Intriguingly, people who are genetically predisposed to Alzheimer's tend to have trouble naturally producing nitric oxide.
In the current study, molecular biologist Joanna L'Heureux and her colleagues found that of 33 participants with MCI who were genetically predisposed to Alzheimer's, many had oral microbiomes dominated by the Prevotella genus and not the Neisseria genus.
One species of Prevotella in particular, P. intermedia, was a predictor for an elevated genetic risk for dementia. This suggests it could be used as an early marker of disease risk.
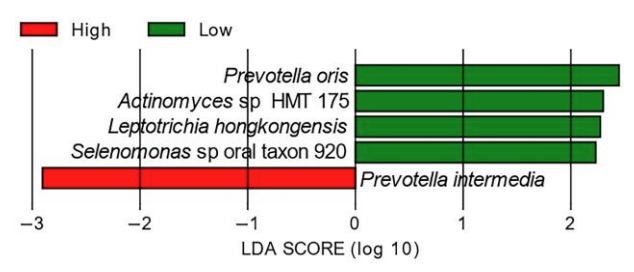
In the study, when the Prevotella genus reigned, there was less nitrate available in the mouth to convert to nitric oxide, probably because Prevotella uses the nitrate for other means.
Thus, by promoting Neisseria and eradicating Prevotella in the mouth, the authors of the study think they could potentially influence nitric oxide availability, thereby influencing the health of the brain.
Nitrate-rich diets, like the Mediterranean diet, are linked to improved brain health, but further research is needed to understand the link between what we put in our mouths, our oral microbiome, and the major signaling molecules produced by those microbes.
A 2021 study in healthy older people, for instance, found a correlation between oral microbiomes dominated by Neisseria (and a co-occurring genus, called Haemophilus) and sustained attention, even when the amount of dietary nitrate changed.
Other research has linked higher rates of Neisseria to younger age, lower body mass index, fewer teeth with damage, and not smoking.
"Collectively, these results indicate that a high relative abundance of bacteria belonging in the Neisseria–Haemophilus module is associated with better cognitive outcomes in individuals with MCI as well as in healthy older people," conclude L'Heureux and her team.
The study was published in PNAS Nexus.
