A landmark study indicates HIV pre-exposure prophylaxis (PrEP) used in everyday life reduces the chances of being infected with the virus by 86 percent.
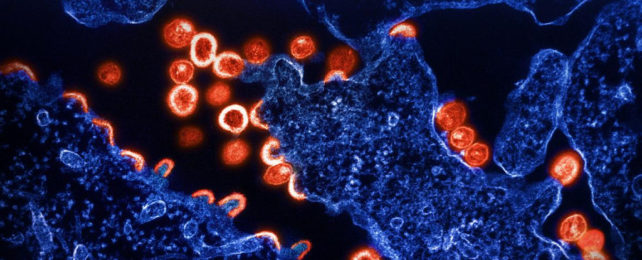
HIV PrEP (commonly referred to simply as PrEP) works by preventing human immunodeficiency virus (HIV) from entering the body and replicating.
Clinical trials have found it to be up to 99 percent effective against the sexual transmission of HIV when taken consistently, at least four times per week.
Now, the most extensive real-world study among participants at sexual health clinics demonstrates that PrEP continues to be effective when administered in everyday healthcare settings without the strict controls of a lab.
Over 24,000 attendees at 157 clinics in England took part in the three-year NHS-funded trial.
"Now we know just how effective PrEP is in real-world settings, substantially reducing the chance of acquiring HIV," says public health scientist John Saunders from the UK Health Security Agency.
"It's vital that all those who can benefit from PrEP can access it."
Participants in the trial were HIV-negative, aged 16 or older, and considered to be at risk of contracting HIV by clinicians. Treatment was prescribed through routine sexual health services from October 2017 to July 2020.
A combination of two existing medicines, tenofovir disoproxil and emtricitabine, the PrEP treatment could be taken daily or 'event-based' before sexual activity.
After various exclusions from the initial sample, the analysis of PrEP treatment effectiveness included 21,356 people.
This sample size was deemed more than adequate for estimating the proportion accepting PrEP treatment among the overall eligible UK population.
"The data support earlier evidence that PrEP is highly effective," the researchers write in their published paper; "incident HIV infections were rare and almost all occurred in the context of having discontinued PrEP."
Scientists are constantly learning more about HIV.
Among rare and difficult-to-confirm 'cures' in people living with HIV, attempts to develop a preventative vaccine, though disappointing so far, are continuing.
Despite being challenging to eliminate once infected, HIV is very treatable and no longer a death sentence.
This confirmation of the efficacy of PrEP in preventing new infections is more positive news and, along with other sexual health measures, might account for the fact that rates of new HIV diagnoses globally are falling.
"PrEP is highly effective in a real-world setting across several years of use," the team explains. "However, further work is required to optimize PrEP delivery to all who could benefit."
The yearly overall number of new HIV diagnoses in England has been steadily decreasing, from 5,780 in 2014 to around 3,000 in 2021.
Although the highest proportion of new HIV diagnoses (36 percent in 2021) are among cisgender gay, bisexual, and other men who have sex with men, this demographic also has the greatest decline, of 77 percent, from 3,200 in 2014 to 721 in 2021.
However, among minority groups and heterosexual people (especially women), the number of HIV diagnoses is on the rise.
"More than half of new HIV diagnoses in the UK are among women, heterosexual men, and transgender, non-binary, and other gender-diverse people," the authors write.
There's under-representation of these population groups in HIV prevention trials, including this one, which the researchers suggest may be attributed to a lack of awareness about sexual health, HIV, and prevention methods like PrEP, as well as stigma associated with both HIV and PrEP.
Infectious diseases physician Ann Sullivan from Chelsea and Westminster Hospital NHS Foundation Trust says the trial has "further demonstrated the effectiveness of PrEP in preventing HIV transmission and has provided key insights, including identifying subgroups where more work is needed."
The study has been published in The Lancet HIV.