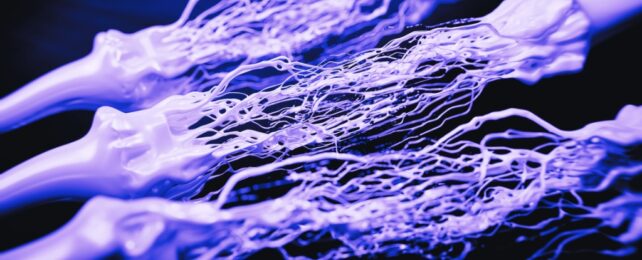
A new study on mice suggests the cause of Alzheimer's disease may not be the buildup of beta-amyloid clumps in the brain but rather breaks in the connections (synapses) between brain cells.
By manipulating the natural processes of RNA editing in mice modelled to reflect Alzheimer's symptoms, researchers prevented the connections in their brains from breaking down. Memory was restored without removing the protein clumps that are thought to cause the disease, suggesting damage between neurons was a critical problem.
The finding provides a new understanding of Alzheimer's disease and an approach that could potentially address memory loss in Alzheimer's patients.
The team is optimistic about developing this process into a viable treatment for humans.
"People living with Alzheimer's experience a loss of these nerve cell connections which has been speculated to cause debilitating loss of memory that is synonymous with the disease," says neuroscientist Bryce Vissel from the University of New South Wales in Australia.
"We now have compelling evidence, in a model of Alzheimer's, that preventing the breakdown in these synapses is possible."
A multi-talented molecule that helps process genetic information, RNA (ribonucleic acid) goes through changes even after it's produced that can affect how it functions.
One of these changes, called RNA editing, involves changing its sequence, which could in turn affect how the protein it encodes works. This editing process happens a lot in the brain and is important for how memories work.
Neurodegenerative diseases, including Alzheimer's disease, have been linked to RNA editing not working properly. In Alzheimer's, changes in memory-related synapses are linked to cognitive decline.
The research showed that there is a specific place to change a protein called GluA2, which is part of a receptor that helps neurons talk to each other. There is evidence that editing happens less at this site in people with Alzheimer's disease, which may contribute to neurodegeneration.
Changing the editing pattern at this site in a mouse model of Alzheimer's disease decreased several symptoms of the disease, such as the loss of neurons, loss of dendritic spines (protrusions from neurons which are essential for synaptic functions), and problems with memory.
So RNA editing, especially at the identified site, may be a key part of how Alzheimer's disease progresses, shedding light on new ways to understand and treat the disease.
"RNA editing can be used as a 'molecular switch'. By flicking the switch in the mice models we use in our research we were able to stop the brain cell connections from breaking down," explains Vissel.
There has also been a longstanding suggestion that imbalances in calcium levels play a role in Alzheimer's. The researchers modified the specific RNA editing process in a way that affects calcium flow in nerve cells and observed positive changes both in healthy control mice and in AD models.
The results suggest that RNA editing plays a role in regulating the structures connecting nerve cells in both healthy and diseased brains. Targeting this specific RNA editing process could potentially enhance the survival of nerve cells and improve memory in Alzheimer's.
"RNA editing worked to restore nerve cell connections without having to remove any amyloid from the animals' brains. This in turn rescues memory, offering a new way forward to understanding and treating the disease," Vissel says.
"Having shown that preventing synapse loss offers a way forward to treating Alzheimer's, our team will now accelerate work towards developing an effective treatment for this devastating disease."
The study has been published in Molecular Neurodegeneration.